Rotavirus gastroenteritis: symptoms, causes, treatment, prognosis
Content
- What is Rotavirus Gastroenteritis?
- ICD-10 code
- Causes of rotavirus gastroenteritis
- Epidemiology
- Pathogenesis
- Symptoms and course
- Complications
- Diagnosis and differential diagnosis
- Rotavirus gastroenteritis treatment
- Forecast
- Prophylaxis
- Individual prevention measures
What is Rotavirus Gastroenteritis?
Rotavirus gastroenteritis (rotavirus infection) Is an acute viral disease with a predominant illness in children; characterized by symptoms of general intoxication, damage to the gastrointestinal tract, dehydration.
ICD-10 code
A08.0. Rotavirus enteritis.
Causes of rotavirus gastroenteritis
The causative agent belongs to the Reoviridae family, the Rotavirus genus. Rotaviruses got their name from Latin rota - a wheel, since viral particles under an electron microscope look like small wheels with a thick bushing, short spokes and a thin rim. The size of viral particles is 65-75 m. They contain RNA.
Human rotaviruses can be cultured in green monkey kidney cells. In terms of antigenic properties, rotaviruses are divided into 9 serological types, of which types 1-4 and 8-9 are found in humans, types 5-7 are isolated from animals. Rotaviruses of animals (dogs, cats, horses, rabbits, mice, calves, birds) are non-pathogenic for humans. Rotaviruses are stable in the external environment.
Epidemiology
The disease is widespread in many countries of the world, accounting for about half of all intestinal disorders in children in the first two years of life in developing countries.
In the United States, more than 1 million cases of severe rotavirus diarrhea are observed annually among children aged 1 to 4 years, in 150 patients the disease is fatal. In 90% of older children, anti-rotavirus antibodies are found in the blood, which indicates a wide spread of this infection.
In some children and adults, the infection can occur inapparently. Immunity is type-specific. In Germany and Japan, antibodies against rotaviruses of serotypes 1 and 3 prevailed. Different serotypes may predominate in the same country over the years. So, in Australia in 1975, rotavirus serotype 3 prevailed, in 1977 and 1978 - serotype 2, and in 1980 and 1986, rotavirus serotype 1 was more often detected.
Children under the age of 3 are more likely to get sick in both developed and developing countries. Rotaviruses are responsible for 30-50% of all cases of diarrhea requiring hospitalization and rehydration therapy. Often, adults in families where the child fell ill also get sick, and elderly people with weakened immunity also get sick.
Rotavirus infection accounts for about 25% of cases of the so-called travelers' diarrhea. Rotavirus infection can be asymptomatic, and such cases are often found in newborns. This course further protects children from severe rotavirus gastroenteritis during the first 3 years of life.
Pathogenesis

Source and reservoir of infection only man is. The causative agent is excreted in feces (1 g of feces contains up to 10-10 viral particles) for up to 3 weeks (usually 7-8 days from the onset of the disease). Infection occurs through the fecal-oral route. The airborne mechanism of transmission of infection has not been proven.
In tropical countries, rotavirus infection occurs year round, with a slight increase in incidence during the cool rainy season. In countries with a temperate climate, seasonality is quite pronounced with the highest incidence in the winter months. A person becomes infected by the alimentary route. Reproduction and accumulation of reovirus occurs in the upper gastrointestinal tract, in particular in the epithelium duodenum. The absence of severe fever and symptoms of general intoxication (in the absence of information about viremia) suggests that the hematogenous route of spread of rotaviruses does not have significant value.
Read also:Hemorrhoids: Causes, Symptoms and Treatment
Rotaviruses cause the death of mature cells of the small intestine, they are replaced by immature absorbing cells, unable to adequately absorb carbohydrates and other nutrients, resulting in osmotic diarrhea.
Intracellular metabolism of cyclic adenosine monophosphate or guanosine monophosphate is not important in the pathogenesis of rotavirus diarrhea.
Rotaviruses accumulate in the intestinal mucosa and then enter the intestinal lumen. Large losses of fluid and electrolytes are pathogenetically important, which leads to dehydration, usually no more than II-III degrees. Small amounts of rotaviruses have also been found in the colon.
Rotavirus infection often combined with other viral (adeno- and coronaviruses) and bacterial (Escherichia, Shigella, Salmonella, Campylobacter) agents. However, rotaviruses themselves can cause damage to the gastrointestinal tract, which has been proven in animal experiments.
Microscopic examination of the mucous membrane of the small intestine reveals areas with a smoothed surface, shortened villi, there is an infiltration of the mucous membrane with mononuclear cells. Rotavirus particles can be detected with electron microscopy. After 4-8 weeks the mucous membrane of the small intestine is completely normalized.
With rotavirus disease, the epithelium of the villi of the small intestine is partially destroyed, in which the synthesis of disaccharidases occurs. As a result, unsplit disaccharides accumulate in the intestine. The process of absorption of simple sugars is also disrupted. All this leads to an excess flow of disaccharides and simple sugars into the colon, which leads to an increase in osmotic pressure. In this regard, a large amount of fluid enters the colon from the tissues, which can lead to the syndrome dehydration. This process is exacerbated by inflammation associated with rotavirus infection.
Immunity to rotavirus infection in most cases occurs in early childhood after an illness. Immunity is unstable, so in adults with low antibody levels, the disease can recur. Immunity in those who have recovered is due not only to humoral, but also secretory antibodies.
Symptoms and course

The incubation period lasts from 15 hours to 7 days (usually 1-2 days). The disease begins acutely. A detailed picture of the disease is formed within 12-24 hours from the onset of the disease. Most hospitalized children body temperature reaches 37.9 ° C and above, and some may rise to 39 ° C and above. In mild forms of the disease, both in adults and in children, severe fever does not occur. Patients note:
- epigastric pain;
- nausea;
- vomiting.
On examination, it is often noted:
- hyperemia of the pharynx;
- signs of rhinitis;
- enlarged cervical lymph nodes.
However, the most typical manifestations of the disease are symptoms of damage to the digestive system.
Characterized by abundant watery watery stool without admixture of mucus and blood. A more severe course is usually caused by a layer of secondary infection. Half of the patients have vomiting.
In adult patients, against a background of moderate intoxication and low-grade fever, pain in the epigastric region, vomiting and diarrhea. Only in some patients, vomiting is repeated on the 2-3rd day of illness. In adults, hyperemia and granularity of the mucous membrane of the soft palate, palatine arches, uvula are often detected, as well as hyperemia of the sclera. Signs of general intoxication are noted only in 10% of the total number of patients, they are weakly expressed.
Read also:Hemochromatosis
All patients have abundant watery stools with a pungent odor, sometimes the feces are unclear-whitish, may resemble the patient's feces cholera.
Loud rumbling in the abdomen is characteristic. The urge to defecate is of an imperative nature, there are no false urges. In some patients, there is an admixture of mucus and blood in feces, which always indicates a combination of rotavirus gastroenteritis with a bacterial infection (shigellosis, escherichiosis, campylobacteriosis). These patients more pronounced fever and general intoxication.
Signs of inflammation of the upper respiratory tract, which are detected in some patients with rotavirus diseases, are considered by some authors to be a consequence of the layering of a secondary viral infection.
With profuse loose stools, dehydration may develop. Dehydration develops quite often (in 75-85% of hospitalized children), but in most cases (in 95%) it is not clearly expressed (I and II degrees of dehydration according to V. AND. Pokrovsky). Only in some cases does severe dehydration develop with decompensated metabolic acidosis. In these cases, it is possible acute renal failure and hemodynamic disorders.
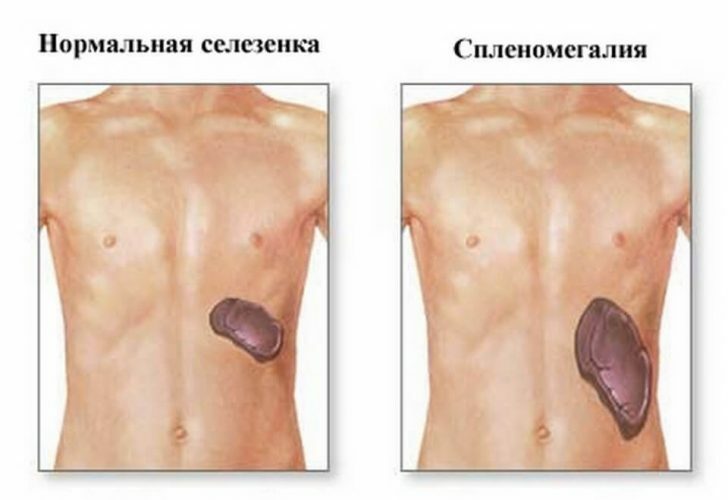
On palpation of the abdomen, pain is noted in the epigastric and umbilical regions, a rough rumbling in the right iliac region. Liver and spleen not enlarged. During sigmoidoscopy, most patients have no changes, only some patients have moderate hyperemia and edema of the mucous membrane of the rectum and sigmoid colon. Signs of damage to the digestive system persist for 2-6 days.
The amount of urine in the acute period of the disease is reduced, in some patients there is albuminuria, leukocytes and erythrocytes in the urine, an increase in the content of residual nitrogen in the blood serum. At the onset of the disease, there may be leukocytosis, which is replaced by leukopenia during the peak period. ESR not changed.
Complications
Rotavirus disease does not give complications. It is necessary to take into account the possibility of a secondary bacterial infection layering, which leads to changes in the clinical picture of the disease and requires a different therapeutic approach. The features of the course of rotavirus infection in persons with immunodeficiencies (HIV-infected, etc.) have not been sufficiently studied. Necrotizing enterocolitis and hemorrhagic gastroenteritis.
Diagnosis and differential diagnosis
When recognizing, the clinical symptoms of the disease and epidemiological prerequisites are taken into account. Characterized by an acute onset, abundant watery stools without pathological impurities with a frequency of up to 10-15 times per day, vomiting, dehydration with a moderate temperature reaction and symptoms of general intoxication. The winter seasonality of the disease, the group nature, as well as the absence of positive findings during conventional bacteriological studies for the intestinal group of microbes are important.
The diagnosis is confirmed by the detection of rotaviruses in stool by various methods (immunofluorescent, etc.). Serological methods are of lesser importance (RSK, etc.). For examination, stool is collected with a sterile wooden spatula in a penicillin bottle (1/4 part of the bottle), secure the rubber stopper with adhesive plaster, deliver to the laboratory in containers with ice.
Differentiate from cholera, dysentery, escherichiosis, gastrointestinal forms of salmonellosis, intestinal yersiniosis, protozoal diseases (giardiasis, cryptosporoidosis, balantidiasis).
Rotavirus gastroenteritis treatment

Treatment is symptomatic, i.e. aimed at combating the symptoms of the disease. In mild cases, oral rehydration therapy (ORT) is used, which is used commercially available means for ORT (rehydron, hydrovit, trihydron, etc.) or solutions of independent cooking.
Read also:Achalasia of the cardia: symptoms and treatment
The simplest solution for oral rehydration therapy is prepared at home. To do this, you need to dissolve 25 grams of sugar (6 teaspoons) and 2.1 grams of salt (half a teaspoon) in a liter of clean drinking water. This simple remedy, recommended by the World Health Organization and UNICEF, can successfully fight dehydration in children.
The resulting solution is given to infants with a syringe or pipette every 1-2 minutes, a few drops. Children over 1 year old are given a teaspoon of the solution every 1-2 minutes. Children of younger preschool age are given a solution in the form of frequent drinking. If the child has vomited, you need to wait 5-10 minutes and then continue to give the solution.
Oral rehydration therapy begins at the first sign of diarrhea and continues until a stable improvement in the condition (no vomiting, loose watery stools).
Oral rehydration therapy is used as first aid. In mild cases, home treatment is possible. If fluid intake is not possible and induces vomiting, urgent medical attention should be sought for intravenous rehydration therapy.
If you have symptoms of intestinal infection, you should try to continue breastfeeding. Breast milk contains all the trace elements and minerals you need, as well as antibodies to help fight infection.
Forecast
The prognosis for rotavirus infection is excellent if adequate hydration is maintained. Most children recover within a week of symptoms.
Rotavirus gastroenteritis has practically no important long-term consequences.
Reinfection (i.e. re-infection) is common.
Prophylaxis
For the primary prevention of rotavirus gastroenteritis, vaccination is used. Vaccine prophylaxis is important only for children and is carried out in the first months of a child's life. Vaccination can reduce the incidence by 50-70% and prevent up to 90% of all severe cases of rotavirus infection in children under 3-5 years old. The effectiveness of vaccination is confirmed by statistical studies in those countries where vaccination against rotavirus gastroenteritis was included in the calendar of mandatory vaccinations for children (reducing the frequency of deaths and morbidity).
In Russia, routine vaccination against rotavirus infection is not used, but it is planned to introduce it by 2019. It can be done privately even now.
Secondary prevention of rotavirus gastroenteritis consists in maintaining proper social conditions and protecting water resources from faecal contamination.
Individual prevention measures
- Maintain personal hygiene, wash your hands before eating and after using the toilet;
- Do not use water from open natural sources without first boiling;
- Do not eat unwashed fruits, vegetables and herbs;
- Try not to eat outside - this is especially true for children;
- When out with your child, use hand sanitizers;
- Use separate utensils and utensils when preparing food for your baby. Sterilize baby drinkers and bottles by boiling or using special devices.