Rehabilitation period after abdominal surgery: regimen and diet
 After any surgical intervention, the patient can not just take it and immediately return to the usual mode of life.The reason is simple - the body needs to get used to the new anatomical and physiological relationships( after all, as a result of surgery, the anatomy and the arrangement of the organs were changed, as well as their physiological activity).
After any surgical intervention, the patient can not just take it and immediately return to the usual mode of life.The reason is simple - the body needs to get used to the new anatomical and physiological relationships( after all, as a result of surgery, the anatomy and the arrangement of the organs were changed, as well as their physiological activity).
A separate case - surgery on the abdominal organs, in the first days after which the patient must adhere strictly to the prescriptions of the attending physician( in some cases - and related consultants).Why, after a surgical procedure on the abdominal organs, does the patient need a certain regimen and diet?Why can not you just take it back to the old way of life?
Table of contents: Mechanical factors negatively affecting the operation Chemical factors negatively affecting the operation Post-operative changes from the intestine Post-operative changes from the side of the skin Postoperative changes on the skin side Post-operative changes on the part of the respiratory organs Post-operative changes on the vascular side Post-operative changesFrom the genitourinary system Diet after abdominal surgery Postoperative activities relatedWith CNS work Prophylaxis of bedsores after surgery Prevention of postoperative pneumonia Prevention of thrombosis and thrombolysis Measures aimed at resumption of normal urination General recommendationsMechanical factors negatively affecting the operation
The postoperative period is considered the length of time from the endSurgical intervention( the patient was taken from the operating room to the ward) and until the time of the disappearance of temporary disordersIn( inconveniences), which are provoked by an operating trauma.
Let's consider what happens during the surgical intervention, and how the postoperative state of the patient depends on these processes and, hence, his regime.
Normally, the typical condition for any abdominal organ is:
- lie quietly in its rightful place;
- is in contact exclusively with neighboring bodies, which also occupy their rightful place;
- perform tasks prescribed by nature.
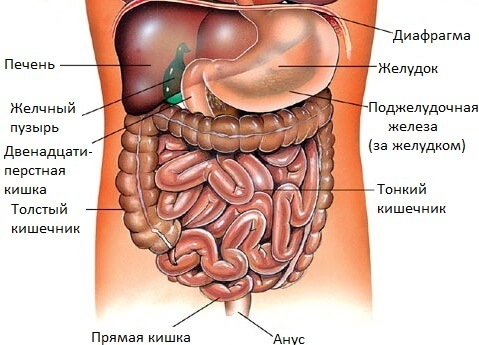
During the operation, the stability of this system is violated. Removing a sore appendix, sewing a perforated ulcer or repairing an injured bowel, the surgeon can not work only with the organ that has fallen ill and requires repair. During surgical intervention, the operating physician contacts constantly with other organs of the abdominal cavity: touches them with their hands and surgical instruments, moves them away, moves them.Let such trauma and reduce as much as possible to a minimum, but even the slightest contact of the surgeon and his assistants with internal organs is not physiological for organs and tissues.
 Mesentery is characterized by a special sensitivity - a thin connective tissue film with abdominal organs connected to the inner surface of the abdominal wall and through which nerve branches and blood vessels approach them. Mesentery injury during surgery can lead to painful shock( despite the fact that the patient is in a state of medical sleep and does not react to irritations of his tissues). The expression "Tear for a mesentery" in surgical slang has even acquired a portable meaning - this means causing severe discomfort, causing suffering and pain( not only physical, but also moral).
Mesentery is characterized by a special sensitivity - a thin connective tissue film with abdominal organs connected to the inner surface of the abdominal wall and through which nerve branches and blood vessels approach them. Mesentery injury during surgery can lead to painful shock( despite the fact that the patient is in a state of medical sleep and does not react to irritations of his tissues). The expression "Tear for a mesentery" in surgical slang has even acquired a portable meaning - this means causing severe discomfort, causing suffering and pain( not only physical, but also moral).
Chemical Factors Negatively Effective During Operation
 Another factor on which a patient's condition depends after surgery is the drugs used by anesthetists during operations to provide anesthesia.In most cases, abdominal cavity operations are performed under anesthesia, a little less often under spinal anesthesia.
Another factor on which a patient's condition depends after surgery is the drugs used by anesthetists during operations to provide anesthesia.In most cases, abdominal cavity operations are performed under anesthesia, a little less often under spinal anesthesia.
In anesthesia, substances are injected into the bloodstream, the task of which is to cause a state of medical sleep and relax the anterior abdominal wall so that surgeons can operate comfortably.But besides this valuable property for the operating team, such drugs have "minuses"( side effects of ).First of all, this depressive( depressing) effect on:
- central nervous system;
- intestinal muscle fibers;
- muscular fibers of the bladder.
Anesthetics, which are injected during spinal anesthesia, act locally, without inhibiting the central nervous system, intestines and bladder - but their influence extends to a certain area of the spinal cord and the nerve endings that leave it, which need some time to "get rid" ofAction of anesthetics, return to the previous physiological state and provide innervation of organs and tissues.
Post-operative changes from the intestine
As a result of the drugs that anesthetists injected during the operation to provide anesthesia, the intestine of the patient ceases to work:
- muscle fibers do not provide peristalsis( normal shrinkage of the intestinal wall, as a resultWhich food masses move in the direction of the anus);
- on the mucosal side, mucus secretion is inhibited, which facilitates the passage of food masses through the intestine;
- the anus is spasmodic.
 As a result - the gastrointestinal tract after the lumbar operation seems to freeze .If at this point the patient takes at least a small amount of food or liquid, it will be immediately ejected from the digestive tract as a result of reflex vomiting.
As a result - the gastrointestinal tract after the lumbar operation seems to freeze .If at this point the patient takes at least a small amount of food or liquid, it will be immediately ejected from the digestive tract as a result of reflex vomiting.
Due to the fact that the medicines that caused short-term intestinal paresis, after a few days will be eliminated from the bloodstream, the normal passage of nerve impulses along the nerve fibers of the intestinal wall will resume and it will start working again. Normally, the bowel function resumes independently, without external stimulation. In the vast majority of cases occur 2-3 days after surgery.The timing may depend on:
- the volume of the operation( how broadly the organs and tissues were drawn into it);
- its duration;
- degree of intestinal injury during surgery.
The signal for the resumption of bowel function is the escape of gases from the patient. This is a very important point, indicating that the intestine has coped with operational stress. It's not for nothing that surgeons jokingly call the departure of gases the best postoperative music.
Post-operative changes from the CNS side
Drugs administered to provide anesthesia are completely removed from the bloodstream after a while. Nevertheless, during their stay in the body they have time to influence the structure of the central nervous system, affecting its tissues and inhibiting the passage of nerve impulses along neurons.As a result, in a number of patients after the operation, there are violations from the central nervous system.The most common:
- sleep disturbance( patient heavily falling asleep, sensitive to sleep, wakes up from the effect of the slightest stimulus);
- tearfulness;
- oppressed state;
- irritability;
- memory violations( forgetting faces, events in the past, small details of some facts).
Post-operative changes from the skin
After surgery, the patient is forced for some time solely in the reclining position. In those places where bone structures are covered with skin practically without a layer of soft tissue between them, the bone presses on the skin, causing a violation of its blood supply and innervation.As a result, the necrosis of the skin - the so-called bedsores - occurs in the place of pressure.In particular, they are formed in such areas of the body as:
-
 sacral spine and coccyx;
sacral spine and coccyx; - scapula( with scoliosis and different bulging of the vanes, pressure sores can be asymmetric);
- heels;
- knees;
- ribs;
- toes;
- large trochanter of femurs;
- stops;
- ischium bones;
- crests of the iliac bones;
- elbow joints.
Post-operative changes on the part of the respiratory system
 Often large cavitary operations are performed under endotracheal anesthesia.For this, the patient is intubated - that is, an endotracheal tube is inserted into the upper respiratory tract, connected to an artificial respiration apparatus. Even with a neat introduction, the tube irritates the mucous membrane of the respiratory tract, making it sensitive to the infectious agent.Another negative aspect of mechanical ventilating during surgery is some imperfection of dosing of the gas mixture delivered from the ventilator to the respiratory tract, and also the fact that the person does not normally breathe .
Often large cavitary operations are performed under endotracheal anesthesia.For this, the patient is intubated - that is, an endotracheal tube is inserted into the upper respiratory tract, connected to an artificial respiration apparatus. Even with a neat introduction, the tube irritates the mucous membrane of the respiratory tract, making it sensitive to the infectious agent.Another negative aspect of mechanical ventilating during surgery is some imperfection of dosing of the gas mixture delivered from the ventilator to the respiratory tract, and also the fact that the person does not normally breathe .
In addition to the factors negatively affecting the respiratory system: after the operation, the excursion( movement) of the chest is not yet complete, which leads to stagnant phenomena in the lungs.All these factors can provoke the emergence of postoperative pneumonia.
Post-operative changes from the vessels
Patients who suffered from vascular and blood diseases are prone to the formation and removal of blood clots in the postoperative period. This is facilitated by a change in rheology of blood( its physical properties), which is observed in the postoperative period.The contributing factor is also that the patient is in a recumbent position for a while, and then begins the motor activity - sometimes abruptly, as a result of which the existing thrombus can be detached. Basically, lower limb vessels are susceptible to thrombotic changes in the postoperative period.

Postoperative changes from the genitourinary system
Often after surgery on the abdominal organs, the patient can not urinate.There are several reasons:
- paresis of the muscular fibers of the bladder wall due to the effects of drugs on them that were injected during the operation to provide medical sleep;
- spasm of the sphincter of the bladder for the same reasons;
- difficulty urinating due to the fact that it is done in an unusual and unsuitable for this posture - lying.
Diet after abdominal surgery
 Until the intestines work, you can neither eat nor drink. The thirst is weakened by applying a piece of cotton wool or a piece of gauze moistened with water to the lips.In the vast majority of cases, the work of the intestine resumes independently.If the process is difficult - inject drugs that stimulate peristalsis( Prozerin ).Since the resumption of peristalsis, the patient can take water and food - but start with small portions. If gases accumulate in the intestine, but can not escape - put the gas pipe.
Until the intestines work, you can neither eat nor drink. The thirst is weakened by applying a piece of cotton wool or a piece of gauze moistened with water to the lips.In the vast majority of cases, the work of the intestine resumes independently.If the process is difficult - inject drugs that stimulate peristalsis( Prozerin ).Since the resumption of peristalsis, the patient can take water and food - but start with small portions. If gases accumulate in the intestine, but can not escape - put the gas pipe.
A dish that is first given to a patient after resuming peristalsis is a lean, thin soup with very little digested cereal, which does not provoke gas formation( buckwheat, rice), and mashed potatoes .The first meal should be in the amount of two to three tablespoons.Half an hour later, if the body does not reject the food, you can give two or three more spoons - and so on, to 5-6 small meals a day.The first meals are not aimed at satisfying hunger, as on "accustoming" the gastrointestinal tract to its traditional work.
Do not force the work of the digestive tract - let the patient stay hungry. Even when the intestine is working, a hasty expansion of the diet and Gastrointestinal Tension can lead to the fact that the stomach and intestines can not cope, this will cause vomiting that, due to concussion of the anterior abdominal wall, will adversely affect the postoperative wound . The diet is gradually expanded in the following order:
- lean soup;
- mashed potatoes;
- creamy cereals;
- soft-boiled egg;
- soaked bread crumbs;
- cooked and ground mashed vegetables;
- steam cutlets;
- unsweetened tea.
Further for 10-14 days the patient must adhere to the dietary food used in the treatment of gastrointestinal diseases - this is an exception to the following types of food:
- oily;
- acute;
- is saline;
- is acidic;
- fried;
- sweet;
- cellulose;
- beans;
- coffee;
- alcohol.
Then the set of dishes is gradually expanded towards the usual diet, which took place in the pre-operative period of the patient.
Postoperative activities related to the operation of the CNS
Changes in the central nervous system due to the use of anesthesia can disappear on their own from 3 to 6 months after surgery. Longer disturbances require consultation of a neuropathologist and neurological treatment of ( often outpatient, under the supervision of a physician). Non-specialized measures are:
- maintaining a benevolent, calm, optimistic atmosphere in the patient's environment;
- vitamin therapy;
- non-standard methods - dolphin therapy, art therapy, hippotherapy( beneficial effect of communication with horses).
Prophylaxis of decubitus after operation
In the postoperative period, pressure sores are easier to prevent than cure. Prophylactic measures should be taken from the very first minute the patient is lying down.It:
- rubbing of risk areas with alcohol( it must be diluted with water so as not to cause burns);
- circles under the places that are prone to the development of pressure sores( sacrum, elbows, heels), so that the risk zones are as if suspended - as a result, bone fragments will not press on the skin;
- massaging tissues in risk zones to improve their blood supply and innervation, and hence trophic( local nutrition);
- vitamin therapy.
If bedsores still occur, they are challenged with:
- desiccants( brilliant green);
- preparations, improving trophic tissue;
- wound healing ointments, gels and creams( panthenol type);
- antibacterial drugs( for the prevention of infection).
Prevention of postoperative pneumonia
The most important prevention of congestion in the lungs is the early activity of :
- whenever possible early lifting from bed;
- regular walks( short, but frequent);
- gymnastics.
If, due to circumstances( a large amount of surgery, a slow healing of the postoperative wound, a fear of postoperative hernia), the patient is forced to lie in a recumbent position, using measures preventing the stagnation in the respiratory system:
-
 Patient inflation of ordinary children's balloons;
Patient inflation of ordinary children's balloons; - vibromassage of the thorax;
- charging at the level of the shoulder girdle( twisting the torso in the sitting position, flexing-unbending arms in the shoulder joints and so on).
Prevention of thrombosis and rupture of blood clots
Prior to surgery of patients aged or those suffering from vascular disease or changes in the blood coagulation system, they are carefully examined - they are made:
- rheovasography;
- coagulogram;
- definition of prothrombin index.
During the operation, as well as during the postoperative period, the legs of such patients are carefully bandaged.During bed rest, the lower extremities should be in an elevated state( at an angle of 20-30 degrees to the plane of the bed).Antithrombotic therapy is also used.Her course is prescribed before the operation and then continues in the postoperative period.
Measures to resume normal urination
 If in the postoperative period the patient can not urinate, resort to the old good trouble-free method of stimulation of urination - water noise.To do this, simply open the water tap in the room to make water come out of it.Some patients, hearing about the method, begin to talk about the dense shamanism of doctors - in fact, these are not miracles, but only a reflex response of the bladder.
If in the postoperative period the patient can not urinate, resort to the old good trouble-free method of stimulation of urination - water noise.To do this, simply open the water tap in the room to make water come out of it.Some patients, hearing about the method, begin to talk about the dense shamanism of doctors - in fact, these are not miracles, but only a reflex response of the bladder.
In cases where the method does not help, the bladder is catheterized.
General recommendations
After surgery on the abdominal organs, the patient is in a lying position in the early days. The time frame in which he can get out of bed and start walking is strictly individual and depends on:
- volume of operation;
- its duration;
- of the patient's age;
- its general condition;
- presence of concomitant diseases.
After uncomplicated and non-removable operations( hernia, appendectomy, and so on), patients can go up 2-3 days after surgery. Large-scale surgical interventions( for breakthrough ulcers, removal of injured spleen, intestinal injuries, etc.) require a longer recumbency for at least 5-6 days - the patient can first be allowed to sit in the bed, dangling his legs, then standAnd only then start to take the first steps.
To avoid the occurrence of postoperative hernias, it is recommended to wear a bandage to patients:
- with a weak anterior abdominal wall( in particular, with untrained muscles, flaccidity of the muscular corset);
- is obese;
- aged;
- to those who have already undergone surgery for hernias;
- recently given birth to women.
Appropriate attention should be paid to personal hygiene, water procedures, ventilation of the room.Weakened patients, who were allowed to get out of bed, but they have a hard time doing it, are taken to fresh air in carriages.
Smokers are strongly advised to quit smoking at least in the postoperative period.
In the early postoperative period, intense pain can occur in the area of the postoperative wound.They are stopped( removed) by anesthetics. It is not recommended to endure the patient's pain - painful impulses re-irritate the central nervous system and deplete it, which is fraught with a variety of neurological diseases in the future( especially in old age).
Kovtonyuk Oksana Vladimirovna, medical reviewer, surgeon, consulting physician