Gangrene lung: symptoms, diagnosis, treatment principles
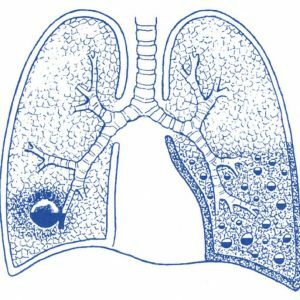 Gangrene of the lung is a purulent-putrefactive process in the lung, which destroys and deadens the lung tissue.Such rotting and necrosis has a tendency to steady spreading and there are no clear boundaries. Gangrene is considered to be the most serious infectious destructive process in the lungs, with this disease a very serious general condition of the patient is noted. With lightning-fast gangrene of the lung, death can occur in the first day of the disease.
Gangrene of the lung is a purulent-putrefactive process in the lung, which destroys and deadens the lung tissue.Such rotting and necrosis has a tendency to steady spreading and there are no clear boundaries. Gangrene is considered to be the most serious infectious destructive process in the lungs, with this disease a very serious general condition of the patient is noted. With lightning-fast gangrene of the lung, death can occur in the first day of the disease.
Among all patients with destructive pulmonary diseases, one in ten suffers from gangrene of the lungs.
Table of contents:Causes of gangrene of the lung
The immediate cause of the onset of this disease is an infection.In most cases, this is not one pathogen, but an association of different microorganisms( including anaerobic - living without oxygen). Most often, gangrene lungs are provoked by such pathogens:
- pneumococcus;
-
 Haemophilus influenzae;
Haemophilus influenzae; - enterobacteria;
- Staphylococcus aureus;
- Klebsiella;
- Pseudomonas aeruginosa;
- fusobacteria;
- bacteroides.
Thanks to this combined action, the microorganisms
- mutually reinforce their virulence( the ability to infect the body);
- are resistant to antibiotics.
In the pulmonary parenchyma, pathogens can get in different ways.The most common:
- bronchogenic;
- aspiration;
- pin;
- is traumatic;
- is lymphatic;
- is hematogenous.
Bronchogenic by , microorganisms enter from the infected oral cavity and nasopharynx through the bronchi into the lung tissue.This is facilitated by the following pathological processes:
-
 tooth caries( cases of gangrene associated with a small imperceptible hole in the tooth enamel are described);
tooth caries( cases of gangrene associated with a small imperceptible hole in the tooth enamel are described); - gingivitis( inflammation of the gums);
- parodontosis( inflammation of tissues around the tooth);
- sinusitis( most often - inflammation of the maxillary sinuses);
- pharyngitis( inflammation of the laryngeal mucosa).
Aspiration path - entry into light fluids containing infectious agents.It can be:
- the secret of the upper respiratory tract - more often it's the usual catarrhal discharge of the nasopharyngeal mucosa);
- contents of the stomach - in most cases such aspiration is observed with dysphagia( swallowing violation), alcohol intoxication, violations of the lower esophageal sphincter, anesthesia, craniocerebral trauma.Sometimes the contents of the stomach enter the lungs with a pronounced eructation or vomiting.
But not all people accidentally inhaling fluid from the upper respiratory tract or stomach lead to infection in the lungs.This often happens when the drainage function of the bronchus is broken, when they can not be cleansed by themselves( for example, when the ciliated epithelium suffers, cilia which normally push out "rubbish" from the bronchi). Often such infection of the lungs occurs against the background:
- blockage of the bronchus with a tumor or foreign body;
- thromboembolism( clogged by thrombus) of the pulmonary artery.
Contact path - is the ingress of microorganisms into the lung tissue from neighboring organs and tissues already infected with . The highest statistics of infection by contact with purulent-inflammatory diseases. First of all it is :
- bronchiectasis( pathological dilatation of the bronchi with subsequent suppuration);
- pneumonia( pneumonia);
- lung abscess( limited abscess in pulmonary tissue).
Traumatic path - penetration of infection into the lung tissue with penetrating chest wounds . In this case, traumatic objects must be infected with microorganisms that can provoke the appearance of gangrene of the lungs.
Lymphogenous pathway pathogens penetrate into the lungs with lymph from already existing infectious foci in the body, by hematogenous - by the same principle, only with blood flow. Lymphogenous and hematogenous pathways of infection of the lung, after which its gangrene develops, most often can be observed in such diseases and conditions as:
- sepsis;
- osteomyelitis( purulent lesion of bones);
- sore throat;
- acute parotitis( defeat of the parotid gland - inflammatory or purulent);
- acute appendicitis( especially often - purulent or purulent-necrotic).
Factors contributing to the onset of the disease
A number of diseases and conditions that do not directly cause gangrene of the lung but cause it to arise:
- depletion and dystrophy that can be observed due to the severe course of many diseases;
-
 operating period after complicated surgical interventions( optional on the respiratory system);
operating period after complicated surgical interventions( optional on the respiratory system); - prolonged bed rest with severe illnesses( not necessarily respiratory system diseases), which leads to congestion in the lungs;
- reception of corticosteroids( for example, with bronchial asthma);
- addiction;
- alcoholism;
- HIV infection;
- old age.More often gangrene of the lung develops in elderly patients who during their life have suffered frequent, long or severe diseases of the respiratory system.
In such conditions, gangrenous lung involvement is most often observed.
How the develops
Having penetrated into the lung tissue and begins to destroy it, the bacteria secrete toxins that enter the bloodstream, and with its current into the tissues of unaffected organs.Also, the products of extensive putrefactive decomposition of lung tissue are absorbed into the blood.
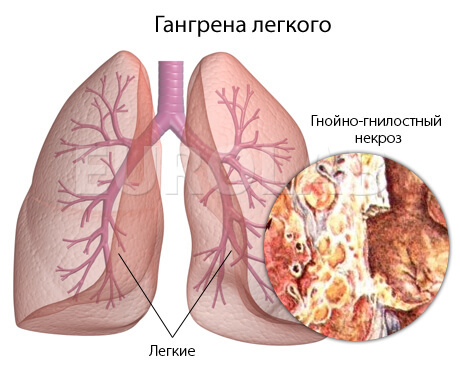
All these substances, which are essentially biological poisons, provoke:
- tissue isolation of substances whose action is directed to stop inflammation are the so-called anti-inflammatory cytokines;
- free radical formation.
Because of the increased production of cytokines and free radicals, the melting of lung tissue is further intensified, the gangrenous process progresses and spreads to healthy lung tissue, and poisoning of the body also increases. A kind of vicious circle is formed, for the exit from which the body's own forces without medicamentous reinforcement are not enough.
Symptoms of the gangrene of the lung
The intensity of the symptoms depends on the vastness of the process - gangrene can spread to one lobe, several lobes of one lung, the whole organ on one side or both lungs.
The manifestations of the disease depend on its shape.There are several such forms: :
- bronchogenic( due to pneumonia, inhalation of fluid or any blockage of the bronchus);
- thromboembolic( as a consequence of blockage of the pulmonary artery);
- is post traumatic;
- gangrene due to the introduction of microorganisms into the lungs from the already existing foci of infection in the body.
Often gangrene in one lung is observed together with an abscess in another.
Depending on the degree of gangrenous destruction of the lung tissue, it can be observed:
- switching off the lung site due to atelectasis( tissue failure);
- necrosis of part of the lung tissue;
- necrosis of small areas of the lung in the form of foci throughout the body;
- purulent melting of necrotic areas of the lung .
All symptoms that signal gangrene of the lung can be divided into several groups, the symptoms of which occur sequentially, group by group.These are the signs:
- inflammation and intoxication;
- lesions of lung tissue;
- respiratory failure;
- bacterial-toxic shock.
Symptoms of inflammation and intoxication with gangrene of the lung:
- increase in body temperature to 39-40 degrees Celsius;
-
 often coming chills;
often coming chills; - intensive sweating - in the patient there is literally a pouring sweat;
- headaches;
- strong weakness, because of which it is difficult to perform even elementary actions - to sit in bed or raise your hand;
- marked absence of appetite and weight loss;
- insomnia;
- in especially severe cases - a violation of consciousness and delirious condition, when the patient does not realize where he is, what happens to him, does not recognize people, starts to delirious, he has visual and auditory hallucinations( less often - olfactory).
Symptoms of lung damage begin to occur after symptoms of inflammation and intoxication:
- observed a painful cough;
- almost immediately begins to withdraw phlegm - fetid, dirty-gray, asphalt color .Sputum, which is secreted with gangrene of the lung, has three characteristic layers during sedimentation in the vessel: the upper one is foamy, with mucus and pus, the middle one with a trace of blood, the lower one - a fine precipitate in the form of crumbs( sand) with scraps of molten lung tissue and pus. Such secretions cleared with a full mouth, for a day the patient can cough up from 0.5 to 1 liter of sputum;
- If there is chest pain from the side of the lesion, which increases when you try to breathe in deeply, this indicates the involvement of the pleura in the gangrenous process and the development of their inflammation.
Signs of respiratory failure are associated with the symptoms described above, when gangrene has melted the lung tissue and the lung does not cope with its responsibilities.These are:
- pallor of the skin;
- cyanosis of fingertips, lips and nose( acrocyanosis);
- shortness of breath with a tendency to build up.
Bacterial toxic shock occurs when the body can no longer cope with gangrene of the lung.Its signs:
- progressive decrease in blood pressure;
- increasing heart rate increase;
- decrease in the amount of excreted urine.
There are no mild forms of gangrene - the course is 100% severe or extremely difficult. Therefore, if on the background of a cough with abundant phlegm and fever the patient feels disgusting - it is necessary to suspect gangrene of the lung.
Complications of the gangrene of the lung
Gangrene is dangerous not only in itself - it can cause complications that can lead to the death of the patient . This is:
- pleural empyema( suppuration of pleural sheets without clear boundaries);
- phlegmon of the chest wall( abscess, more and more spreading to soft tissues);
-
 pericarditis( inflammation of the heart's "shirt"), including purulent;
pericarditis( inflammation of the heart's "shirt"), including purulent; - pneumothorax( due to destruction of the lung tissue, the pleural cavity, in which the normal pressure is normally filled with air from the respiratory tract);
- severe pulmonary hemorrhage;
- sepsis with ( general infection of the body with an infectious agent that has entered the vascular bed) and its variety of septicopyemia( the formation of secondary abscesses due to the fact that the infectious agent has got into the blood and with its current spread throughout the body);
- DIC-syndrome( mass formation of thrombi in small vessels);
- respiratory distress syndrome, or "wet lung"( severe respiratory failure due to pulmonary tissue infiltration);
- multiple organ failure( when several important organs cease to perform their functions).
With gangrene of the lung, such complications cause death of patients in 45-80%.
Diagnosis of gangrene of lung
The general severe condition of the patient with increasing disturbances on the part of the respiratory system( especially cough with a large amount of fetid sputum) and pronounced hyperthermia makes it possible to suspect gangrene of the lung.
Such patients have a very characteristic appearance:
- are inactive, which is very evident;
- skin of a characteristic pale-earthy hue;
- lips, fingers, sometimes the tip of the nose is cyanotic.
When coughing up patients can hear loud gurgling sounds.
Additional diagnostic methods should be undertaken:
- to clarify the location and extent of the gangrenous process in the lung;
- in extremely rare cases, when the reactivity of the organism suffers, and the clinical symptoms lag behind in their manifestation from the gangrenous process in the lung tissue, which managed to go far.
 Of the additional instrumental diagnostic methods, the most important application is lung radiography in two projections - X-ray machines are even available in a small hospital.
Of the additional instrumental diagnostic methods, the most important application is lung radiography in two projections - X-ray machines are even available in a small hospital.
The radiograph shows extensive dimming - signs of the cavity of decay and fluid in the pleural cavity( the latter indicates a transition of the process to the pleura and warns of impending deterioration in the general condition of the patient).In most cases, chest radiography is sufficient to confirm the presence of spreading disintegration in the lungs provoked by gangrene.
Fluids in the pleural sinuses can also be detected using ultrasound of the pleural cavity.
Computed tomography makes it possible to determine the initial foci of necrosis scattered throughout the surface of the lung - this will help diagnose gangrene in its early stages, which is important for treatment.
Also the patient gives phlegm for her microscopic examination of .In it, with gangrene, leucocytes, erythrocytes, necrotic fragments of lung tissue are detected in a large number, and the absence of elastic fibers is ascertained. In order to identify the pathogen and clarify its sensitivity to antibacterial agents, bacteriological culture is done:
- phlegm;
- lavage fluid, which is obtained by rinsing the upper respiratory tract for the purpose of sanitation.
Bronchoscopy is performed in order to clarify whether there is purulent endobronchitis ( inflammation of the bronchial mucosa), which can develop due to the entry of pathogens from gangrenous pulmonary foci into both small bronchi and higher into large ones.
A general blood test will confirm a pronounced inflammatory process -
- will show a sharp increase in the number of leukocytes with a predominance of neutrophils;
- increased ESR( ESR);
- anemia.
In the expanded blood test, the following is determined:
- a reduced amount of protein, the reserves of which the organism "throws" on attempts to restore damaged lung tissue;
- decrease in the amount of oxygen;
- increase in the amount of carbon dioxide.
Treatment of gangrene of the lung
Treatment of gangrene of the lung is a very difficult task, which is solved jointly by pulmonologists and thoracic surgeons with the use of consulations.
All treatment measures include:
- conservative treatment( drug therapy);
- sanitation procedures;
- surgical treatment.
Conservative treatment consists of the following activities:
- antimicrobial therapy, which is central to conservative treatment;

- detoxification of the body( excretion of the products of lung disintegration and vital activity of gangrene pathogens);
- correction of disturbances of homeostasis( stable internal environment of the body);
- restorative therapy.
For the purpose of antimicrobial action, combination of two broad-spectrum antibacterial agents is used in the maximum possible dosages. Antibiotics are administered in different ways:
- parenterally( intravenously and intramuscularly);
- topically( into the bronchial tree and into the pleural cavity).
Detoxification of the body is due to intensive infusion therapy. Intravenous drip is introduced:
- low-molecular solutions - plasma substitutes;
- saline solutions;
- Protein preparations( albumin);
- whole blood and its components( plasma, and in case of anemia - erythrocyte mass).
To correct for homeostatic disorders, the following preparations are used:
- vitamins;
- anticoagulants;
- respiratory analeptics;
- desensitizing agents;
- cardiovascular drugs;
- immunomodulators.
Conservative, non-drug methods are also used:
- oxygen therapy that helps saturate tissues with oxygen until the affected lung does not cope with this function;
- plasmapheresis( collection of blood from the bloodstream, purification in special devices and introduction back into the bloodstream);
- inhalation with bronchodilators and enzymes that dilute hard-to-separate sputum.
As with gangrene of the lung the body is very weak, restorative therapy is no less important than other conservative treatments:
- strict bed rest;
- balanced quality food with emphasis on products containing proteins and vitamins( regardless of parenteral administration of protein and vitamin preparations);
- in the period of improvement - feasible motor activity;
- adequately matched massage.
In order to act directly on the gangrenous focus, therapeutic bronchoscopies are used, during which:
- aspirates the detachable bronchi and the decay products of lung tissue;
- is used to flush the bronchi with antiseptics;
- is administered antibiotics.
If pleurisy develops - perform a pleural puncture, during which:
- aspirate pleural exudate;
- in the pleural cavity is injected with antibiotics.
 If the diagnosis of gangrene of the lung was made in the early stages of the disease, when there was no pronounced necrosis of the tissues, and intensive conservative therapy was scheduled in time, it is possible to stop the destruction of the lung tissue and help to limit it in the form of a gangrenous abscess.
If the diagnosis of gangrene of the lung was made in the early stages of the disease, when there was no pronounced necrosis of the tissues, and intensive conservative therapy was scheduled in time, it is possible to stop the destruction of the lung tissue and help to limit it in the form of a gangrenous abscess.
With further dissemination of gangrene, the patient is first prepared using these conservative methods, and then surgery is performed to remove the affected part of the lung( up to removal of the entire organ if it is completely affected).In some cases, due to the technically unavailable removal of dead tissues, a pneumotomy is performed, a drainage operation, through which the dead tissue will be excreted outward.At the same time, intensive conservative treatment is continuing to completely stop the spread of the process.
Prevention
Prevention of gangrene of the lung is a very difficult task. Prevention of this disease is effective when directed not only to prevent the infection of potential causative agents of the gangrene . The complex of measures includes:
- general health education of the population, especially in the regions;
- improvement of living standards;
- campaign for a healthy lifestyle and against bad habits;
- the correct organization of medical measures for bacterial diseases( in particular, purulent-septic).
- sepsis;
- multiple organ failure;
- blood loss due to massive pulmonary hemorrhage.
Despite the fact that patients with gangrene of the lung are promptly undergoing surgical treatment, supported by conservative methods, the mortality rate remains high - 20-40% of patients with gangrene die, most often from complications such as:
Cure a patient of gangrene and prevent its consequences with a timely diagnosis and adequate treatment.
Kovtonyuk Oksana Vladimirovna, medical reviewer, surgeon, consulting physician



