Spiral intrauterine
 The intrauterine device spiral is an artificially created synthetic device for the purpose of insertion into the uterine cavity to prevent the development of an unplanned pregnancy. Modern intrauterine spirals differ in appearance( loop, umbrella, ring, spiral, T-shape, etc.) and material( plastic, copper, silver and others) from which they were made. They do not cause discomfort or pain to women, they are relatively easy to inject and remove. Since the first products, which received the widest application, were made in the form of a spiral, the term "spiral" is now often used as a habit to call contraceptive products of any shape.
The intrauterine device spiral is an artificially created synthetic device for the purpose of insertion into the uterine cavity to prevent the development of an unplanned pregnancy. Modern intrauterine spirals differ in appearance( loop, umbrella, ring, spiral, T-shape, etc.) and material( plastic, copper, silver and others) from which they were made. They do not cause discomfort or pain to women, they are relatively easy to inject and remove. Since the first products, which received the widest application, were made in the form of a spiral, the term "spiral" is now often used as a habit to call contraceptive products of any shape.
The intrauterine hormone spiral( Mirena and analogues) is very popular among modern specialists. In addition to the usual contraceptive effect, she copes with hormonal dysfunction and prevents the development of certain diseases.
Attempts to use intrauterine contraception date back to ancient times. The first scientific substantiation of this technique refers to 1909 and belongs to Richter, who proposed to insert into the uterine cavity a ring made of biological material - the intestine of a silky worm. In 1926 the German scientist Grafenberg proposed his version of an intrauterine contraceptive - a ring made from an alloy of metals. However, all proposed devices, when administered, injured uterine tissue and often provoked unwanted complications. The problem of creating a more suitable material for making an intrauterine contraceptive was decided only in 1960 by the American scientist Lips, when he suggested using a more elastic material. Since the product suggested by him looked like a loop, he was called a "Lips loop".
Intrauterine contraception, if properly used, approaches the efficacy of 100%, thus comparable to the use of hormonal birth control pills. Like any medical technique, intrauterine spirals have both significant advantages and disadvantages.
Let's start with the advantages. In addition to high efficiency, intrauterine devices have other advantages:
- Guaranteed expected effect without additional efforts. When using hormonal contraception, it is necessary to monitor the intake of the drug, sometimes even a once-missed tablet can cause unwanted pregnancy. Spiral also guarantees the contraceptive effect continuously, including the menstrual period.
- The cost of one package of oral contraceptives is much less than the cost of a single spiral, however, from an economic point of view, the use of a spiral is cheaper, because hormonal tablets need to be bought monthly, and the spiral can be in the uterus up to five years.
- Non-hormonal spirals relieve a woman from the unwanted consequences of contraception in the form of hormonal dysfunction. Since they do not interfere with the natural hormonal background, they are absolutely safe for those who are breastfeeding and those women who have categorical contraindications for taking oral contraceptives.
- The intrauterine device Mirena( or similar), in addition to the contraceptive, also has a therapeutic beneficial effect: it restores the hormonal background, prevents local inflammation, reduces menstrual blood loss.
- The mechanism of action of the usual intrauterine device does not imply a change in the hormonal background, therefore, unlike oral contraceptives, does not inhibit ovulation. After the extraction of the spiral from the uterine cavity pregnancy may occur in the near future. This advantage can not boast of hormone-containing spirals, since the restoration of fertility after their evacuation from the uterus in terms comparable to that after the abolition of hormonal contraceptive pills.
- Intrauterine contraception does not cause systemic metabolic disturbances.
- The presence of a copper, silver or gold component in the spiral suggests an anti-inflammatory effect.
The ubiquitous use of intrauterine contraception is limited, as, like any other technique, it has several drawbacks, namely:
- The introduction of an intrauterine device is not always shown to nulliparous young women. Since the opening of the external pharynx in nulliparas is tightly closed, and the cervical canal is narrow enough, the introduction of the spiral is very difficult.
- As the threads of the spiral "descend" into the vaginal cavity, the outer pharynx remains slightly ajar at first, which in turn makes the cervical canal and uterus vulnerable to potential infection. Often women who change their sexual partners using intrauterine contraception have a high risk of developing infectious inflammation.
- The uterine musculature responds to the presence of a spiral in all women in different ways. Sometimes, in order to adapt to a foreign body and not try to push it out, the uterus takes a long time, which explains the moderate pain in the projection of the uterus. As a rule, they disappear in the first year after the introduction of the spiral.
- Virtually everyone using an intrauterine device spiral notes an increase in menstrual blood loss. If the monthly becomes too abundant, especially with the development of anemia, the spiral must be removed.
- The intrauterine device is not able to protect the genital tract from infection, especially sexually transmitted infections.
- Under certain conditions, especially if the woman does not follow the advice given by the doctor, the intrauterine device can leave the uterine cavity on its own. The frequency of expulsion( fallout) of spirals is low, but this possibility must be taken into account.
Introduction of the intrauterine device, as well as its removal, is carried out only by a specialist, and every woman is able to control the delivered spiral independently.
Thus, intrauterine contraception is a worthy competitor to hormonal, not yielding to it on efficiency and safety. Since each of these techniques has pros and cons, the right choice can be made by a specialist.
Principle of operation of the intrauterine device
Before discussing the prevention of conception, it is necessary to recall how it occurs. Every month, a small "vial" appears in the ovary with a fluid - the follicle. It contains an egg. While the egg does not "grow up" and will not be ready for fertilization, the follicle feeds it and protects it from negative external influences. In the put period( the period of ovulation), the follicle releases an egg, and itself collapses. The ovum that falls outside the ovary is caught by the fallopian tube and begins to move toward the uterine cavity, waiting for the sperm to meet and then fertilize. If fertilization does not occur, the egg dies within 24 hours.
So, the egg ripens in the ovary, then it enters the fallopian tube, where it fertilizes after meeting with the spermatozoon, and then moves to the uterus for implantation.
Despite the fact that the technique of intrauterine contraception is used and improved for many decades, there is no single view of the mechanism of its action. The most reliable are several theories of contraceptive action of the intrauterine device, namely:
- Theory of abortive action. It is based on the assumption that the intrauterine contraceptive induces the rejection of a fertilized egg in the womb.
- Theory of aseptic( noninfectious) inflammation. Asserts that the presence of a spiral provokes in the endometrium structural changes that do not involve the development of pregnancy. Mucous uterus perceives a spiral as a foreign body and responds to its presence by immunological reactions that provoke a local inflammatory process of an aseptic property.
- Theory of acceleration of peristalsis of fallopian tubes. The lining of the uterine tubes of the epithelium( ciliated) has a unique structure: its cells have special thin "cilia", capable of making wave-like movements( flicker).Twinkling of the epithelium allows the ovum to move in the proper direction, that is, towards the uterine cavity. If the fallopian tubes peristalticize too quickly, the egg "in transit" does not have time to "ripen" correctly and therefore can not be implanted into the endometrium.
- The theory of spermatotoxic effects. The copper and silver found in the spiral affect the motor activity of spermatozoa and prevent them from reaching the fallopian tubes.
Thus, the intrauterine device can affect the egg in two ways:
- do not let it "meet" with sperm for fertilization;
- prevent the implantation of a fertilized egg into the endometrium.
Apparently, one can not give preference to only one theory explaining the action of the intrauterine device. It is more logical to assume that each of them has the right to exist, because it explains only one of the mechanisms of the "work" of the contraceptive in the uterus.
Types of spirals of intrauterine devices
Among modern intrauterine contraceptives, one can find "spirals" made of a wide variety of materials. They are made on the basis of medical, biologically compatible, plastic( polyethylene) with the addition of copper, silver, gold. It is also possible to add hormones to the helix.
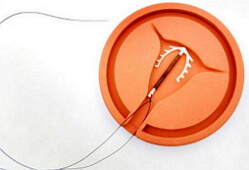
The shape of the spiral, regardless of the material of manufacture and cost, must be physiological, that is, have this shape and size to fit the size and shape of the uterine cavity. Often they have the shape of an oval, rings, letters T or S, and dimensions not exceeding 3x4 cm. Long threads( "whiskers") are a mandatory attribute of any intrauterine device. If the body of the contraceptive is to be located in the uterine cavity, then its strings necessarily run in the cervical canal and are partially located in the vagina.
All available intrauterine contraceptives are divided into:
- Non-ametable, which, in addition to the contraceptive, do not have an additional( eg, anti-inflammatory) effect. These are inert( neutral) products made of biologically safe and flexible plastic with the addition of barium sulfate. In recent years, when there are more modern intrauterine contraceptives, this group of spirals is used infrequently.
- Medicamentous, consisting of metals or hormones( gestagens).The additional therapeutic effect of the intrauterine device of this group is based on the fact that in a constant rhythm it releases into the uterine cavity the ions of copper, silver, gold or gestagen. Simultaneous presence of only one or several metals is possible when the spiral shaft has one metal( for example, the intrauterine device with silver), and the rest - copper. Containing silver and other metals spirals do not corrode, are able to prevent local inflammation, therefore, they are administered for a long( up to five years) period. The presence of an additional medicamentous component favorably affects the epithelium, reduces the risk of undesirable side reactions, which explains their higher efficacy.
Most experts recommend for intrauterine administration:
- T Cu 380 A - intrauterine T-shaped spiral, including copper ions. Most active against spermatozoa( "immobilizes" them).The presence of copper ions in the epithelium of the uterine cavity also has an anti-inflammatory effect. A great advantage of copper spirals is the possible period of their use - in the womb they can be up to 5 years.
- Multiload Cu 375( or Multiload) - copper-containing semi-oval intrauterine spiral with peculiar protrusions on the periphery resembling small thorns. Such a construction helps the contraceptive to securely fixate in the mucous membranes.
- IUD spiral with silver and / or copper: Nova-T( Nova-T), T de Plata 380, NOVAPLUS( Novaplus) - T-shaped intrauterine contraceptives with plastic, copper and / or silver.
- Gold intrauterine device T de Oro 375 Gold. It has a core made of 99/000 gold. Despite the good anicorrosion properties, copper and silver eventually begin to break down with organic acids present in the mucous membranes. The gold intrauterine device is able to withstand the destructive effect of acidic medium, therefore it lasts much longer( up to 10 years), which justifies its high cost.
- Spiral intrauterine hormonal. Today in the domestic pharmacy network there are two types of such spirals - Mirena( produced by the German company Schering) and Levonov( from the Finnish company Leiras).Mirena is used more often, so the effect of hormonal contraceptives can be discussed on its example.
Intrauterine spiral Mirena has a combined mechanism of action - contraceptive and hormonal. In its composition there is a hormone levonorgestrel, able to cope with large menstrual blood loss, menstrual pain and hyperplastic process. Mirena is introduced according to the indications, not only as a contraceptive, but also as a remedy.
Which intrauterine device is better than
Often, women have difficulty in choosing an intrauterine contraceptive, because the modern medical industry offers many different in form, composition and cost of spirals. More often such a choice helps to make a specialist, however it is necessary to understand that the concept of "good intrauterine spiral" does not exist.
The contraceptive effect of the intrauterine device is its sole purpose, and, since all modern spirals have such a property, any of them can be called "good."
It is much more correct to look not for "the best", but for the most individually tailored intrauterine device. To do this, it is necessary to undergo the examination recommended by a doctor beforehand to exclude the presence of inflammatory diseases, to determine the size and position of the uterus and cervix. In some situations, when a doctor considers the use of an intrauterine device as contraception in a particular patient inexpedient or even dangerous, the use of other contraceptive methods is discussed.
Regardless of the quality and efficiency of the spiral, it can not be administered only at the patient's request. The use of intrauterine contraceptives, like any other medical intervention, is regulated by rules that provide for indications and contraindications.
So, who should refrain from using intrauterine contraception?
First of all, this method is not offered to nulliparous. Due to anatomical features, the introduction of a spiral through the "nulliparous" genital tract is impractical, and the presence of a "foreign body" in the uterine cavity in such women in terms of the degree of the negative effect surpasses the advantages of this type of contraception. Similar reasons do not allow to recommend an intrauterine device to adolescents.
The presence of infectious inflammation at any stage of development excludes the possibility of using an intrauterine device as a contraceptive.
It is not recommended to use an intrauterine device for women with a large number of sexual partners, even if they have no signs of an infectious inflammatory process. After all, this category of patients always has a high risk of developing a specific inflammation, so for them the barrier method of protection against pregnancy, and at the same time - from sexual infections is more acceptable.
The use of an intrauterine device for true and false( ectopic) cervical erosions, tumors of various genesis is also contraindicated.
Thus, a "good intrauterine spiral" should, in the first place, correspond to several mandatory requirements: to provide a high contraceptive effect, not to have a negative effect on the body and not to have contraindications for use.
How is the installation of the intrauterine device
Single-handedly to decide the issue of contraception, in addition to the barrier, is inappropriate. Previously, any woman, even considering herself healthy, should receive the expert's advice and undergo an appropriate examination, which often includes:
- A detailed interview with the patient. Sometimes already at this stage, the introduction of an intrauterine device is not recommended. For example, if the woman is nulliparous, or indicates a significant menstrual blood loss.
- Gynecological examination. Excludes the presence of local inflammation, pseudo-erosion.
- Laboratory diagnostics( bapsoseve, smears, PCR diagnostics and others) to exclude infectious processes in mucous membranes.
- Colposcopy. As a rule, it is recommended after a visual examination of the cervix, if there is a suspicion of pathology.
- Ultrasonic scanning of small pelvis. Helps determine the status of the ovaries, location, size of the uterus, as well as to study the structure of the endometrium. Diagnoses fibroids and polyps. It is not required by everyone, and is conducted according to the testimony.
There is no consensus on the favorable time of intrauterine device administration. Experts believe that this manipulation is not limited to a time frame, and the spiral is allowed to enter any day of the menstrual cycle. Among practical practitioners there is an opinion that intrauterine contraceptive is easier to install on such days when the external throat and, accordingly, the cervical canal are slightly ajar, and the mucous membrane of the uterine cavity is less vulnerable to trauma. Therefore, for the introduction of the spiral, usually the period of the end of menstruation, or its last days( 4-8 days of the cycle) is chosen.
A significant advantage of the intrauterine device is the possibility of its installation after the interruption( artificial or voluntary) of pregnancy. If the patient has signs of inflammation or bleeding, the procedure for administering the contraceptive is postponed until the first after the interruption of menstruation.
Women are often interested in the possibility of introducing a spiral at the end of labor. Indeed, the introduction of an intrauterine device after delivery( subject to the absence of contraindications) is possible and is carried out within the first 48 hours. However, since the uterus has not yet passed the stage of postpartum involution( recovery), the probability of spontaneous spiral expulsion remains high. If the spiral was not injected in the first two days, the procedure for its installation is postponed for one or a month and a half.
Any intrauterine device is introduced exclusively by a specialist. The procedure does not take much time and the majority, in addition to minor discomfort, does not cause unpleasant sensations. Since the installation of the spiral does not imply the instrumental expansion of the cervical cavity, as it is done before the abortion, this manipulation is not accompanied by severe pains, except when the patient experiences severe fear and involuntarily spasms of the muscles.
The doctor must necessarily "probe" the uterus: inserts a special sterile umbilical into the uterine cavity through the cervical channel. This procedure is necessary to make sure that there are no obstacles to the introduction of the spiral, to determine in which direction the contraceptive should be administered, and also to measure the size of the uterine cavity.
The spiral is placed in the syringe - a long thin tube with a piston. It is injected gently through the cervical canal into the uterine cavity, and then the spiral is ejected by means of a piston.
As already mentioned, any intrauterine device has long strands. When it enters the uterus, these strands remain in the syringe and, after it is carefully removed from the cervical canal, remain hanging from the opening of the external throat. The control threads allow the gynecologist to see that the spiral is in the uterus when viewed, and the woman can be sure of the same if she feels for the vagina during hygiene procedures. Contrary to fears of some patients, the control strings are not physically sensed and do not interfere.
Why does a woman need to periodically "check" the spiral? One of the negative consequences of the intrauterine device is its spontaneous prolapse. As a rule, such a situation provokes excessive physical activity, aggressive intimacy. If the spiral expulsion occurred during the period of menstrual bleeding, a woman may not notice it, as it will simply come out with blood. The absence of control threads may indicate a lack of a spiral.
It should be noted that the number of cases of spontaneous expulsion of the intrauterine device has significantly decreased after the emergence of spirals of a new generation, which have the most physiological form and are capable of well "gaining" in the uterine cavity.
After the intrauterine device has been inserted, the doctor makes recommendations to the patient. They must be performed for the first five days. Often a woman is asked not to perform heavy physical work and not to attend the gym, to observe intimate hygiene, to refrain from sexual intimacy, to perform douching or to insert vaginal tampons. According to the indications for this period, a short course of antibiotic therapy can be prescribed.
The presence of a spiral in the uterine cavity may affect subsequent menstruation. It is considered normal, if the monthly become slightly more abundant.
Like any medical manipulation, the introduction of an intrauterine device can provoke negative consequences. At the time of the introduction of the contraceptive, it is possible to damage the tissues of the cervix and uterus, as well as their infection.
The most frequent long-term complications are bleeding, severe pain and inflammation.
As a rule, the negative consequences associated with the intrauterine device are observed infrequently.
Removal of the intrauterine device
Remove the intrauterine device for several reasons:
- if the recommended period of use has expired;
- if a woman no longer wishes to be protected in this way;
- if pregnancy is planned;
- if there is a menopause;
- if an arbitrary partial expulsion occurred;
- in the presence of medical indications: pregnancy, pain, significant bleeding, infectious inflammation.
It is easier to remove the intrauterine device during menstruation, when menstrual bleeding is most pronounced, and the cervical canal is maximally "open".With the help of tweezers, the control threads are grabbed and, gently pulling on them, remove the spiral.
Generally, the extraction of the intrauterine device does not cause serious difficulties. They arise only in those situations when the spiral, contrary to the recommendations of specialists, was in the uterine cavity for too long and "ingrowing" into the endometrium. If attempts to extract it in the usual way are unsuccessful, resort to laparoscopy to find and pull out the contraceptive under visual control.
After removal of the intrauterine device, the patient is recommended to follow the same rules as for her administration.
It should be recalled that the contraceptive effect of the intrauterine device ends immediately after it is removed. Therefore, if the onset of pregnancy is undesirable, it should be timely to think about its prevention.


