Paraovarian ovarian cyst
 Paraovarian cyst of the ovary is a fluid-filled, cavity-filled benign formation located near the ovary. With the body of the ovary, the parovarial cyst is not anatomically connected, but located near it and the fallopian tube, can affect their function. In turn, the functional or structural disorders that occur in the appendages also affect the condition of the cyst.
Paraovarian cyst of the ovary is a fluid-filled, cavity-filled benign formation located near the ovary. With the body of the ovary, the parovarial cyst is not anatomically connected, but located near it and the fallopian tube, can affect their function. In turn, the functional or structural disorders that occur in the appendages also affect the condition of the cyst.
A paraovarian ovarian cyst is classified in a group of so-called retention cysts, they are formed due to accumulation of fluid by any cavity formation. In the ovary, the follicle( follicular cyst) or the yellow body formed in its place( luteal cyst) can be such.
The parovarial cyst of the ovary is located not in the ovary, but near it - between the sheets of the wide uterine ligament, which simultaneously fixes the appendages and uterus. It is formed from the epididymis - parovarium( paraophorone).This education is only a rudiment of the organ that has long lost its value( rudimentary), in fact it is absolutely not necessary for the female body. Paraovarium is a network of small non-functioning tubules that merge into a larger canal. Topographically, it is located between the fallopian tube and the ovary and, since it is underdeveloped, there is no excretory duct.
The cyst of the ovarian appendage is formed by the accumulation of fluid and the overstretching of the walls of the dysfunctional duct, so there is always only one cavity( chamber) inside it. It should be noted that it only has signs of a true cyst, but in fact it is not. With true cysts, it is "related" to the presence of the wall and the liquid contents. The capsule of any true cyst is always thick, consists of a group of cells capable of dividing and providing the growth of the cyst itself. Paraovarial cyst has a different mechanism of development: it grows slowly as the serous fluid accumulates and the walls of the parovarium expand, which is the "capsule".The walls of such a cyst are thin, transparent, formed by cells that are not capable of dividing. Another clinically significant feature of the parovarial ovarian cyst is its absolute good quality.
The cyst of the ovarian appendage can appear as a result of a violation of the correct tissue differentiation during embryonic development, in which case it is classified as congenital. It is also capable of forming with the participation of some provoking factors - inflammatory processes, dyshormonal disorders, traumatic manipulation.
As the paraviarium reaches its greatest development during the period of development and the heyday of the hormonal function, most cases of diagnosis of parovarial cysts occur in the period of 20 to 40 years, and this diagnosis can occur more rarely in girls 8-10 years old. Sometimes the small fossa of the ovarian appendage does not manifest itself clinically and is diagnosed accidentally, in other cases it can slowly increase.
Since the paraovarian ovarian cyst can behave ambiguously, its clinical manifestations are different. Cysts large( more than 5 cm) provoke pelvic pain on the side of localization and dysfunction of adjacent organs.
The paraovarian cyst of the right ovary is neither anatomically nor clinically different from that on the left.
Diagnosis of the parovarian cyst of the ovary is assisted by ultrasound. Sometimes the true localization of the cyst is differentiated badly, and it is taken for the ovarian cyst. However, such a situation is not classified as a significant diagnostic error, since most cysts in the appendage area are subject to surgical removal, and the scope of the operation is always specified on-site.
Paraovarian ovarian cyst does not regress independently. Similar situations are rare, and all of them are associated with a diagnostic error. Removal of paraovarian ovarian cyst is recommended in situations where its diameter exceeds two centimeters, and / or there is a pronounced clinical picture. Preference is given to minimally invasive techniques, more often such is laparoscopy paraovarilany ovarian cyst, which allows you to simultaneously diagnose and remove the cyst.
Causes of paraovarian ovarian cyst
Paraovariast cysts are diagnosed much less often( 10-12%) of follicular and luteal cysts. It provokes the appearance of parovarial cysts premature sexual development, and after 45 years they practically do not occur. This type of cyst, as already mentioned above, begins to form at the stage of embryonic development as a result of local disturbance of tissue differentiation.
The initially formed ovarian adenoma cyst has small( 0.5 - 2.0 cm) dimensions, is filled with a small amount of fluid and is asymptomatic. In this condition, it can be present without development for many years, so it is diagnosed accidentally during ultrasound scanning.
Despite the possible long asymptomatic course, the further behavior of the paraovarian cyst, like the nature of its growth, is unpredictable. Sometimes it begins to rapidly inflame the fluid and increase, provoking a vivid clinic. It is generally believed that stimulating the growth of parovarial cysts is capable of:
- endocrine pathologies, especially pronounced hyper- or hypofunction of the thyroid gland, diabetes;
- chronic menstrual dysfunction accompanied by serious hormonal disorders;
- sluggish undiagnosed infectious-inflammatory processes of the pelvic cavity;
- repeated traumatic situations: abortions, spontaneous abortions, incorrect diagnostic manipulations;
- obesity or, conversely, a significant deficit in weight;
- Irrational long-term use of hormonal drugs, especially contraceptives;
- inadequate thermal effect on the pelvic area( hot baths, solarium, long stay in the hot sun, improper use of mud and warming applications).
These factors( alone or in combination) can sometimes stimulate the growth of the parovarial cyst, but this situation is not necessary.
Symptoms of Paraovarian Ovarian Cyst
In the absence of provoking factors, the parovarial ovarian cyst grows very slowly in the vast majority of cases. The small size of the cystic cavity allows the formation to be present in the body asymptomatically, and the first subjective sensations appear when it increases to five or more centimeters. Paraovarian cysts can reach gigantic sizes, but more often they "stop" by 15 to 20 cm.
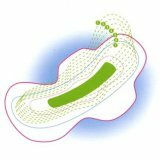
Microscopically, the ovarian adenocast cyst looks like a round or oval formation with a uniform transparent content of a watery appearance. Since the cyst grows solely due to the accumulation of serous fluid and the dilatation of the duct, its walls are very thin( not thicker than 1-2 mm), which makes them look transparent.
A small paraovarian ovarian cyst does not have a leg. As she grows, she pushes the sheets of the broad ligament and forms a protrusion in one of them, pulling the part of the fallopian tube behind her, and sometimes her own ovarian ligament. Thus, the foot of the parovarial cyst is formed.
The enlarged cyst of the ovarian adnex exerts mechanical pressure on adjacent structures and nerve fibers, therefore provokes pelvic pain. Their intensity directly depends on the size of the cyst. A distinctive clinical feature of these pains is the lack of connection with the monthly cycle.
The topography of the pains provoked by the paraovarian cyst is also related to its size and direction of growth. As a rule, the formation is found on the side of the uterus, so the paraovarian cyst of the left ovary provokes pain on the left, and the right cyst provokes the pain on the right, respectively. Often, the cyst appears in the zone above the uterus and exerts mechanical pressure on adjacent organs, then on the background of pain, dysuric disorders occur( if the organs of the urinary system are squeezed) or violations of defecation and a feeling of swollen bowels( under pressure on the rectum).
Usually a small paraovarian ovarian cyst does not affect menstrual function and does not interfere with conception and childbirth. However, in case of intensive growth, it inevitably begins to put pressure on the ovary and provoke menstrual irregularities.
Also, a large cyst of Paraovar sometimes deforms the fallopian tube, so there are problems with conception. Infertility paraovarian cyst of the ovary does not provoke, since structural disorders are formed only on the developmental side of the cyst and do not affect the other, "healthy" half. The patients retain the reproductive function, but the probability of conception decreases slightly. So, for example, the paraovarian cyst of the left ovary does not affect ovulation and subsequent fertilization on the opposite, right, side and vice versa.
Like any cyst that has a thin base( stem), the parovarian ovarian cyst can be complicated by its partial or total torsion. The wall of the cyst, like her leg, is permeated with a variety of blood vessels and nerve endings. When there is a twist, the cyst ceases to "eat", and it starts the process of necrosis, there are all the signs of acute surgical pathology. For example, a paraovarian cyst of the right ovary with a twist of the base mimics the clinic of acute appendicitis.
Treatment of paraovarian ovarian cyst
The choice of treatment strategy depends on the specific clinical situation and the survey data. Initially, it is necessary to establish exactly where the cyst is localized, its structure, size and position relative to neighboring organs.
A large diagnostic value is the size of the parapet. Sometimes lean patients come to the reception after they have personally probed a large formation( and sometimes paraovarian cysts grow to 30 cm) in the projection of the ovary or even saw it with the naked eye.
An experienced physician may already suspect the presence of a parovarial cyst at the initial diagnostic stage even in the absence of active complaints. When palpation from the side or above the uterus, a smooth, densely-elastic formation is defined, limited in mobility. If the patient does not have menstrual irregularities, as well as the association of pelvic pain with the cycle, it can be assumed that this detected formation is topographically located outside the ovary, but any conclusion based on examination and analysis of complaints is only an assumption and needs clarification.
It is possible to differentiate the paraovarian cyst with ultrasound scanning. An important, and perhaps the only distinguishing feature is its location outside the ovary. Other echo signs of the ovarian adenoma cyst are:
- a thin wall with a well-visualized vascular pattern;
- the only cavity( chamber) inside the cyst;
- transparent homogenous( anechogenous) liquid inside the chamber without large inclusions, the presence of fine dispersed suspension is acceptable;
- Parietal papillary growths can be visualized in children inside paraovarian cysts.
After the topography and the size of the cyst are established, a therapeutic tactic is chosen. Small asymptomatic cysts do not require urgent removal, so their behavior can be observed with the help of ultrasound.
Unfortunately, it is often difficult to correctly locate the detected cyst difficult, so the patient is diagnosed with ovarian cysts, and to clarify the diagnosis, laparoscopy is performed on the paraovarian ovarian cyst.
Large symptom parovarial cysts must be removed. There is a large list of surgical techniques, each of which is designed for a specific situation and is selected "on site".Thanks to laparoscopic surgery, removal of the parovarial cyst of the ovary is carried out as sparing as possible, the ovary and uterus are not affected, and the number of complications is practically reduced to zero.
Special attention should be paid to the fact that in no other way the removal of the parovarial cyst is possible, since it is anatomical rather than functional. This cyst is also not capable of self-dissolving.
Operation with paraiovarian ovary
To remove the parovarial cyst of the ovary, it is necessary to penetrate into the place of its location - the fiber of the interconnected space, select the cyst( that is, cut off its capsule from the surrounding tissues), and then remove it from the capsule( enucleation of the cyst).These manipulations often do not cause significant difficulties, since the parovarial cyst is sufficiently mobile. At the next stages of the operation, measures are taken to stop bleeding and prevent septic effects.
The laparoscopic method is often used. If the diagnosis is doubtful, and the localization of the cyst( in the ovary or nearby) remains unknown, diagnostic laparoscopy of the paraovarian ovarian cyst is also curative: after specifying the location of the cyst, it can be removed immediately.
If a parovarian ovarian cyst is diagnosed in a pregnant woman, the treatment strategy depends on the current clinical situation. Pregnancy is not an indication for the urgent removal of the parovarial cyst. Of course, the most desirable is the situation when the pregnant women planning pregnancy pass the examination in advance and solve the problems. But if the presence of a cyst of the ovarian appendage is found already during pregnancy, there is no reason for panic. Small parovarial cysts are located outside the uterus and appendages, do not shift or deform them, and also do not affect the hormonal function. Therefore, their behavior is simply observed, and after the birth the question of the need for treatment is decided. The exception is infrequent cases of complications( necrosis, torsion), which require urgent intervention. It provokes the growth of parovarial cyst pregnancy is infrequent. In such a situation, it is also necessary to operate the patient.
After laparoscopic removal of the paraovarian cyst, pregnancy continues to develop normally, and there are no negative consequences for the fetus.
Paravarian cysts never recur and are not transformed into malignant formations, so after their removal, patients with similar diagnosis or its negative consequences do not face.