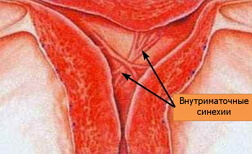
Intrauterine synechiae
 Intrauterine synechia is a spike between individual sections of the uterine mucosa, which leads to its complete or partial infestation. There are several theories about the mechanisms of formation of intrauterine synechia, but the leading place belongs to the mechanical trauma of the epithelial layer of the endometrium, aggravated by the attachment of a secondary infection. Most spikes in the uterine cavity are diagnosed in the first four weeks after a complicated abortion( 67%), childbirth or diagnostic curettage, that is, if the integrity of the epithelium lining the uterine cavity is compromised.
Intrauterine synechia is a spike between individual sections of the uterine mucosa, which leads to its complete or partial infestation. There are several theories about the mechanisms of formation of intrauterine synechia, but the leading place belongs to the mechanical trauma of the epithelial layer of the endometrium, aggravated by the attachment of a secondary infection. Most spikes in the uterine cavity are diagnosed in the first four weeks after a complicated abortion( 67%), childbirth or diagnostic curettage, that is, if the integrity of the epithelium lining the uterine cavity is compromised.
Also intrauterine synechiae are sometimes formed against a background of endometritis, a "frozen" pregnancy, after operations on the uterus or because of the presence of an intrauterine device.
In response to trauma or infectious inflammation in the endometrium, thin connective tissue bands are formed. At first they look like thin, delicate films, and then turn into dense strands that tighten the walls of the uterus.
The mucosal lining layer( endometrium) consists of three unequal cell layers: 25% of the total thickness of the endometrium occupies the basal layer, 50% is functional, and the remainder( 25%) belongs to the middle layer of epithelial cells. Each of these layers has some distinctive structural features and performs a specific function, but all of them are closely related to the common circulatory system and are designed to provide normal fetal and childbearing.
Basal, internal, the layer does not respond to cyclic hormonal fluctuations. It is distinguished by the presence of elastic and connective tissue fibers, which give the endometrium the greatest strength, elasticity and extensibility.
Functional, external, epithelial layer is hormone-dependent. It contains a large number of blood vessels and glandular structures. Symmetrically cyclic hormonal fluctuations according to the phases of the menstrual cycle, this layer changes the cellular composition and thickness. In the first half of the cycle under the influence of estrogens, the functional layer grows and sprouts with a large number of vessels. When the dominant effect of estrogens ends( second phase), the functional layer begins to gradually separate from the uterine wall and is completely eliminated from the uterine cavity during menstruation.
Located between the basal and functional middle endometrium layer will perform the function of the transition zone and contains the cellular elements inherent in both layers. After the end of menstruation, the cells of the inner and middle layer participate in restoring the integrity of the uterine cavity surface.
The source of formation of intrauterine synechia is the basal layer. In fact, their formation is similar to the adhesive process in any hollow organ with mucous lining.
The clinical picture of synechia in the uterus depends on how much the uterine cavity is deformed, from the density and number of adhesions. Sometimes the presence of intrauterine synechia does not cause active complaints and is diagnosed accidentally. Among the complaints of patients with intrauterine synechia are menstrual disorders and infertility.
Intrauterine synechia and pregnancy - a combination of unfavorable, with a high probability of complications in the process of gestation, childbirth and after them.
Diagnosis of intrauterine adhesions is possible only by instrumental means, the most reliable of which is considered hysteroscopy.
Remove intrauterine synechiae only by dissection.
Causes of intrauterine synechia
The most reliable hypothesis of the appearance of adhesions in the uterine cavity remains the traumatic theory, according to which the expansion of the synechia occurs after a significant mechanical injury of the basal layer of the endometrium. The role of infection as a cause of intrauterine synechia is considered secondary.
In response to mechanical damage, the epithelium of the basal layer tends to restore the former integrity and grows exponentially, involving the muscle and fibrous fibers in the process. Specific strands are formed, consisting of cellular structures inherent in the basal and underlying layers. In their composition, soft and flexible elastic collagen fibers or "coarse" connective tissue can predominate. Over time, the synechia "pulls" the walls of the uterine cavity and significantly deforms it. In more severe cases, the uterine cavity can completely close, and the endometrium collapse.
Depending on the structure of intrauterine synechia due to which cellular structures, several types are distinguished:
- Light synechia. Remind thin film, very "tender" and fragile. Formed mucosa of the basal layer.
- Medium-sized synechia. In addition to epithelial cells, they contain denser fibers of fibrous and muscular tissue.
- The densest, heaviest, the synechia. They are formed by a coarse connective tissue.
The most dangerous in terms of the appearance of intrauterine synechia is considered the first month after childbirth or abortion, since it is at this time that active restoration of the endometrium occurs against the background of a vast wound surface. Each subsequent scraping of the uterine cavity increases the risk of intrauterine synechiae appearance by 8%.
Most cases of intrauterine synechia formation are registered among patients after scraping for a "frozen" pregnancy. After the uterine cavity is freed from the deceased embryo, small fragments of placental tissue remain in it, it becomes the source of adhesions formation before the end of physiological regeneration of the endometrium.
If the injury of the endometrium is complicated by an infectious inflammation, an inflammatory exudate is involved in the formation of intrauterine synechiae. It accumulates, becomes more viscous, dense, forms strands and "glues" the uterine cavity. Among the causes of intrauterine synechia of infectious origin is tuberculosis infection.
Symptoms and signs of intrauterine synechia
The clinical picture of the adhesive process in the uterine cavity depends, first of all, on the amount of synechia, their type( light, medium or heavy) and localization. The degree of infection of the uterine cavity affects the manifestations of the disease and determines the success of the therapy. It is therefore extremely important to determine the prevalence of intrauterine synechiae.
I degree. It differs in small( less than 25% of the area of the endometrium) spread of adhesions. As a rule, intrauterine synechiae are thin, resemble films, not localized in the bottom and mouths of fallopian tubes.
II degree.25 - 75% of the uterine cavity is involved in the pathological process. The walls of the uterus are free, the adhesions do not "glue" them, but may partially overlap the bottom of the uterus and the mouth of its tubes.
III degree. It differs by a significant( more than 75%) involvement of the endometrium in the adhesion process. The synechiae are dense and inelastic, capable of significantly deforming the uterine cavity and fusing the uterine walls with each other.
Any intrauterine synechia deforms the uterine cavity, so the disease is almost always accompanied by menstrual irregularities. In connection with the decrease in the area of the functional layer of the endometrium, menstruation becomes meager, hypomenstrual syndrome is formed, and in more severe cases, the menstrual period stops altogether( amenorrhea).
If only the lower part of the uterine cavity is partially overgrown and the endometrium continues to function normally, menstrual blood is evacuated untimely. Therefore, the monthly ones come with delays and last longer, in the form of scant dark discharge. If the uterine cavity in the lower part is completely overgrown, menstrual blood remains in the uterus, and a hematometer is formed.
In addition to menstrual dysfunction, the patient is noted for pain in the projection of the uterus of varying intensity.
Significant infection of the uterine cavity, a decrease in the area of the normally functioning endometrium prevent normal implantation of the fetal egg. In the case of intrauterine synechia localization in the zone of the fallopian tube mouths, fertilization becomes impossible. Infertility is observed in 60% of patients having a synechia in the uterus.
Simultaneously, existing intrauterine synechia and pregnancy lead to a negative scenario. Pregnancy is prematurely interrupted by early( miscarriage) or late( premature birth) timing. Intrauterine synechia provokes the pathology of placenta development: it can grow to the uterine wall. Because of the high risk of not tolerating a child, it is better to plan a pregnancy after dissecting intrauterine synechia.
It is impossible to diagnose the presence of synechia in the uterus on the basis of anamnesis and examination, since their clinical manifestations are non-specific and similar to the symptoms of other diseases.
The most reliable diagnostic method for intrauterine synechiae is hysteroscopy. The synechia is visualized in the form of whitish strands of varying thickness, length and density, which are located between the walls of the uterus, in the cervical canal. The gentle intrauterine synechia resembles a cobweb, they are thin, pale pink, with vessels that can be seen inside. The coarser sineches are devoid of blood vessels, dense, white, stretch along the lateral walls of the uterus and significantly deform its cavity.
In partial occlusion of the uterine cavity, multiple dense transverse strands are visualized during hysteroscopy, they form many apertures, indentations and small cavities.
If the adhesion process captures a significant part of the uterine cavity, hysteroscopy does not allow a detailed examination. In this situation, a more complex technique is used - hysterosalpingography. A contrast medium is introduced into the uterine cavity. It fills the uterus and cavities of the fallopian tubes and well "stains" their contents on X-rays. The method allows you to see how much the uterine cavity is spliced or deformed, and also to determine the presence of synechia in the fallopian cavities.
Treatment of intrauterine synechia
The only way to eliminate intrauterine synechia is by their mechanical dissection. As a rule, the first stage of treatment is performed during diagnostic hysteroscopy, when the spikes found in the uterine cavity are dissected with the help of surgical instruments intended for this technique under the indispensable visual control. If the uterus is pristenochnye tight fusion, they are removed with an acute curette.
The easiest way is to eliminate light synechiae having a film consistency. Delicate splices collapse after touching the tip of the hysteroscope. The middle, fibro-muscular intrauterine synechia after bleeding is bleeding.
Severe intrauterine synechiae, formed by a coarse connective tissue, does not bleed, but dissect with difficulty.
Any procedure for removal of synechia requires repeated hysteroscopic control. If the control examination of the uterine cavity after treatment shows that the synechia is no more, and the corners of the uterus where the fallopian tube mouths are located are free, the treatment is considered successful.
Unfortunately, even the highest quality surgical removal of intrauterine synechia does not exclude the recurrence of the disease. In 60% of the widespread dense synechia "return".Eliminate such a scenario is sometimes helped by the introduction of an intrauterine device( Lips-type loop) for at least one month.
The dissection of the intrauterine synechia treatment does not end. It is necessary to restore the normal structure and functioning of the endometrium, for which resort to cyclic hormone therapy for 3-6 months.
If intrauterine synechiae form on the soil of the infectious inflammatory process, treatment should be supplemented with appropriate antimicrobial therapy.
Pregnancy after intrauterine synechia dissection may occur relatively quickly, but such a scenario, contrary to the opinion of patients, is not successful. In order for a potential pregnancy to develop correctly and result in timely deliveries without complications, it is necessary to completely restore the endometrium, eliminate the infectious component and recreate the correct hormonal function.



