Vulvit and his treatment
 Vulvitis is an inflammation of the external female genital organs. The most common is in childhood and the elderly, because it is during these periods that the mucosa is the most vulnerable and is not capable of providing itself with natural protection. Pain, itching and burning accompany the entire period of the disease, but it becomes especially acute when irritating factors, such as urination and movement, are acted upon.
Vulvitis is an inflammation of the external female genital organs. The most common is in childhood and the elderly, because it is during these periods that the mucosa is the most vulnerable and is not capable of providing itself with natural protection. Pain, itching and burning accompany the entire period of the disease, but it becomes especially acute when irritating factors, such as urination and movement, are acted upon.
Features vulvitis
should understand that this process is not local, but is diffuse distribution pattern, namely affects all the mucous surfaces, can even go inside the vagina and amaze even the hymen. The most important thing is that for such a disease there is no specific pathogen and it is not necessary to have neither contact nor a domestic way of infection from the carrier. Bacteria that cause such a disease, there are in each organism and are considered conditionally pathogenic. This means that they have every person and are usually safe for life, but if you just forget about personal hygiene or lowered immunity, how immediately the development of the inflammatory process begins. Therefore, often people are simply at a loss how this could happen. But not always vulvitis can be triggered by streptococci, staphylococci and E. coli, sometimes it can be a manifestation of gonococcal infection, chlamydia or trichomonas.
Factors contributing to the development of vulvitis:
- Violation of rules of personal hygiene, which means not only timely bath, but also closely synthetic underwear, and the constant wearing pads, rough mechanical damage that hoarding bacterial flora
- Unprotected sexual acts entailing woundsAnd trauma, for example, microcracks
- Systematic exposure to the vulvar mucosa with discharge from the cervical canal with infectious microflora or regular urination irritation, for example, in weeksYerzhan
- chemical burns, especially because here the mucous so gentle that it is sufficient and weak
- solution As a result of long-term treatment with antibiotics or when used bolus
- radiotherapy or radiological loads exceeding the permissible radiation dose
- People with diseases that impair blood circulationsuch as diabetes or obesity
- Hormonal disorders
- Fistulas abdominal and pelvic
Classification vulvitis
Primary - arises itself SEBE as a result of mechanical injuries or reduced immunity. The genitalia of children and women who are in postmenopause are most often affected. But among women of medium or childbearing age this type of pathology is extremely rare, which is due to the protective mechanisms of the reproductive system, providing strong local immunity. In children, most often, a disease caused by worms that cause constant itching in the genital mucosa, and as a result of scratching lesions occur in the form of micro-cracks and scratches, which promote inflammation. As for the period of postmenopause, there is a completely different mechanism of occurrence. Because the mucosa becomes more vulnerable to infection, as it begins to atrophy in view of a change in the hormonal background and a decrease in local immunity, and the amount of secretions from the cervical canal becomes an order of magnitude smaller or disappears altogether, which causes dryness of the epithelium.
Secondary - occurs against the background of an already existing infectious disease, which can be either in the genitals or in completely different ones. For example, inflammation of the tonsils can lead to vulvitis. With this kind of age does not matter. The only thing that predetermines the risks is the prevalence of the underlying disease and the organ that is susceptible to infection, that is, if the uterus or its neck is bacterially affected, the rate and severity of infection to the external genitalia will be more intense than if the bladder or kidney is affected. As a rule, inflammation of the vulva contributes to the presence of infection in the internal genital organs, because the inflammation simply migrates outside.
Clinical picture of
Symptomatology will be different for different types of flow of the process, as it will be more aggressive in the acute phase, and in the case of chronic wavy flow. Of course, for the first time the disease that has arisen will always have an acute course, but if it is not treated effectively or in insufficient volume, it easily passes into a chronic condition and reminds oneself at the first opportunity.
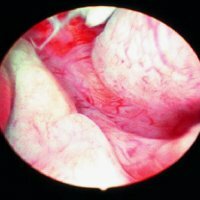
In acute incision, the vulva is swollen, which is characterized by swelling, hyperemic to burgundy shades, and the integrity of the mucosa is disturbed and ulceration and eroded areas appear. Constant itching, burning and pain make a woman's life just unbearable. Before the inflamed area it is even painful to touch, not to mention the movements that increase friction and increase the swelling. With acts of urination and defecation, the already intense pain intensifies even more. As it should be, according to medical aspects, any inflammation is accompanied by general symptoms of inflammation, such as general malaise, fever, body aches, weakness, etc. Literally a few days after the onset of the disease, the discharge from the mucosa becomes not only serous, but purulent. The color can be completely different, because it is caused by the bacterial flora, and each microorganism has its own characteristics. For example, the E. coli secretes not only yellow or green mucus, but also a sharp putrefactive odor.
In chronic course, almost all symptoms persist, but they are not so intense. Swelling and redness weakly expressed and can be local, excretion and itching are minor, do not bother much, but nevertheless cause irritability and build-up due to the constant character.
The disease can go on to the chronic form only if it is acute or if the symptoms disappear, discontinue treatment. But the chronic course of cure is much more difficult. Moreover, the symptoms will still remain, and with the next decrease in immunity or poor-quality hygiene, there will be exacerbations with all the vivid manifestations.
Diagnosis and treatment of vulvitis
If you have these symptoms or suspect them immediately, you need to see a doctor gynecologist, because the clinical picture can grow very quickly, for example, literally overnight, the genital area can become very red and swollen, which will greatly affect normal life activity. Of course, the doctor will immediately prescribe the treatment, but in order for it to be as effective as possible, it will be necessary to take a smear and make a tank seed that will determine the microflora. After all, for each kind of pathogens there is an active substance.
The first thing to observe is maximum rest, if possible, then bed rest, because excess friction and mechanical effects on the affected mucosa are not only sharply painful, but also not desirable. And of course, we should completely exclude sexual acts, because this will greatly aggravate the course of the disease.
As for the medical treatment, everything here depends, as it was said above, on the microflora. But antibiotics are shown in almost all cases, so until the tank is ready for sowing, you can start with ointments or tablets of a wide spectrum of action. The spectrum of drugs is very large, but there are the most common: Polizinaks, Ginezol, Terzhinan, Betadin, etc. but it is not necessary to focus only on the genitals, concomitant diseases, too, should be treated immediately, for example, if there is tonsillitis or pyelonephritisBe taken simultaneously with the main treatment.
Local therapy is of great importance, because it will not only relieve puffiness and eliminate such unpleasant symptoms, but will also speed up the recovery process as a whole. Compresses from soothing decoctions such as calendula or chamomile, with the addition of menthol or eucalyptus, as a cooling effect, will be very handy. With this disease, you should not disregard the old folk methods, because they are simply necessary. One of the most remarkable methods of unofficial medicine are baths with decoctions of oak bark, chamomile or something else with a similar effect, and the effect is reflected both at the local level and on the state of the organism as a whole.
After recovery, the hygiene of the external genitalia should be closely monitored and the gynecologist regularly visited. Timely diagnosis is the key to successful treatment!