Hemangioma of the spine
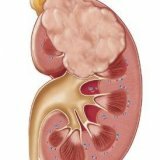
 Hemangioma physicians refer to vascular tumors, occurring in 1-1.2% of cases of all bone tumors. Hemangioma can develop in any of the spine, more often in the thoracic, less often in the lumbar, extremely rarely in the sacral. Usually one vertebra is affected. Among patients with hemangioma, women over the age of 40 predominate.
Hemangioma physicians refer to vascular tumors, occurring in 1-1.2% of cases of all bone tumors. Hemangioma can develop in any of the spine, more often in the thoracic, less often in the lumbar, extremely rarely in the sacral. Usually one vertebra is affected. Among patients with hemangioma, women over the age of 40 predominate.
Types of hemangiomas
By its structure, hemangiomas are divided into the following types:
- cavernous;
- capillary;
- mixed hemangioma.
 By localization, they are divided into the formations located in the body of the vertebra( such a majority), in the arch or processes of the vertebra. Very rarely hemangioma is a soft-tissue component in the vertebral canal, compressing the spinal roots and spinal cord.
By localization, they are divided into the formations located in the body of the vertebra( such a majority), in the arch or processes of the vertebra. Very rarely hemangioma is a soft-tissue component in the vertebral canal, compressing the spinal roots and spinal cord.
In its clinical course, hemangiomas are aggressive( about 10%) and non-aggressive. Most hemangiomas are not life threatening, do not cause any symptoms and are identified accidentally during an MRI or CT scan of the spine. Such formations do not require treatment.
Diagnosis of hemangioma
In most cases these formations are asymptomatic and can be identified by chance during radiographic or neuroimaging studies. Rarely, hemangiomas can cause pain on the background of a pathological fracture. The aggressiveness of hemangioma can be identified only by clinical signs and radiographic findings. The most frequent symptom of hemangioma is a pronounced, permanent, localized pain. Conduction of palpation and percussion of the spinous process and paravertebral area, as a rule, causes pain.
 In the diagnosis of hemangioma, the patient is shown urgent consultation of a neurosurgeon for additional diagnosis( MRI, CT) and determining the need for surgical treatment. Indication for surgical intervention is determined by a neurosurgeon on the basis of the overall clinical picture and studies.
In the diagnosis of hemangioma, the patient is shown urgent consultation of a neurosurgeon for additional diagnosis( MRI, CT) and determining the need for surgical treatment. Indication for surgical intervention is determined by a neurosurgeon on the basis of the overall clinical picture and studies.
Danger of existence of hemangioma
A hidden problem associated with hemangioma can be the "risk of a pathological fracture."A person can not feel any unpleasant symptoms. However, during the examination of the spine, the lesion of nonaggressive hemangioma is determined by more than 50% of the entire vertebral body. This means that even with small loads( running, jumping, falling from a small height), a vertebra affected by a hemangioma can break down.
The insidiousness of such a fracture is that the patient himself sometimes can not tell when exactly he happened. Often a fracture of the vertebral body "captured" by the hemangioma is accompanied by neurological disorders. They are due to compression of the spinal cord. There may be paralysis of the legs or a violation of urination.
Treatment of the hemangioma of the vertebra
 Earlier, radiation treatment was used to treat patients with hemangiomas. Nowadays the main method of treatment is percutaneous puncture vertebroplasty. This is a minimally invasive radiological procedure that consists in the percutaneous injection of polymethyl methacrylate( bone cement) into the damaged vertebral body. Thus, the body of the vertebra is artificially strengthened. The procedure is performed under local anesthesia under compulsory X-ray control.
Earlier, radiation treatment was used to treat patients with hemangiomas. Nowadays the main method of treatment is percutaneous puncture vertebroplasty. This is a minimally invasive radiological procedure that consists in the percutaneous injection of polymethyl methacrylate( bone cement) into the damaged vertebral body. Thus, the body of the vertebra is artificially strengthened. The procedure is performed under local anesthesia under compulsory X-ray control.
In the presence of vertebral hemangioma and compression fracture in the presence of osteoporosis, the risk of complications clinically manifested does not exceed 1%.In the course of the procedure, complications can be associated with the expiration of cement. Expiration is more common in the destruction of the end plates in the back of the vertebral body.
Postoperative period
Within an hour after the procedure, strict bed rest should be observed. Bone cement in this period reaches 90% of its maximum hardness. If visible complications after surgery are not observed, within an hour the patient may be allowed to sit in bed with the help of an assistant.
Control spondylography of the treated level is necessarily performed after the procedure to assess the condition of bone cement. As a rule, in the first few hours after the procedure, the pain syndrome regresses by 50%, but in rare cases, pain can be increased. With increasing pain, the use of non-steroidal anti-inflammatory drugs and analgesics is indicated for 1-2 days.