Diabetic retinopathy - eye damage in diabetes mellitus
 Diabetes is cunning not only in itself.It causes a number of complications that significantly reduce the quality of life.One of these complications is eye damage.In diabetes mellitus, impaired vision occurs due to the destruction of the mesh membrane.It is irreversible, requires long persistent treatment, and in neglected cases it leads to blindness.
Diabetes is cunning not only in itself.It causes a number of complications that significantly reduce the quality of life.One of these complications is eye damage.In diabetes mellitus, impaired vision occurs due to the destruction of the mesh membrane.It is irreversible, requires long persistent treatment, and in neglected cases it leads to blindness.
Diabetic retinopathy - what is it?
 Diabetic retinopathy is included in the "troika" of diseases that are most of all attended by oculists.With this disease, the retina vessels of the eyeball suffer. Their anatomical and physiological disorders are caused by elevated blood sugar levels.If a decade ago, diabetic retinopathy in most cases excruciated older patients( from 50 years and older), but now it is rapidly "younger", and doctors are no longer surprised at the cases of eye vascular disease in diabetes in patients aged 23-28 years.
Diabetic retinopathy is included in the "troika" of diseases that are most of all attended by oculists.With this disease, the retina vessels of the eyeball suffer. Their anatomical and physiological disorders are caused by elevated blood sugar levels.If a decade ago, diabetic retinopathy in most cases excruciated older patients( from 50 years and older), but now it is rapidly "younger", and doctors are no longer surprised at the cases of eye vascular disease in diabetes in patients aged 23-28 years.
The longer a person suffers from diabetes, the greater the percentage of probability that diabetic retinopathy will kill him.
In patients with diabetes mellitus diagnosed for 5-7-10 years, diabetic changes in the retina of varying severity are observed with a frequency of 45% to 80% of dispensary cases, and more than 15 years - from 87% to 99%. A total of diabetic retinopathy is susceptible, according to various data, to 85-90% of patients suffering from diabetes, regardless of the duration of the disease.Complaints for visual impairment in this disease in the vast majority of cases appear after its long flow. This is a kind of hint in the diagnosis - loss of visual acuity in the early stages of diabetes mellitus speaks about:
- concomitant pathology, which should doubly alert the ophthalmologist, because such a disease will also progress because of diabetes mellitus;
- less often - on the rapidly developing in the tissues of diabetic changes that cause deterioration of the eyes, this affects the correction of treatment.
If you do not engage in a patient, then, inevitably worsening your vision, diabetes sooner or later leads to blindness, which is actually a synonym for disability. Loss of vision in patients with diabetes occurs 25 times more often than in cases of blindness caused by other causes.According to different data, a total loss of vision suffers from 2% to 5% of those suffering from diabetic retinopathy.Most people meeting you on the street wearing sunglasses tapping their wand are blind because of a "sweet" illness.
Causes of retinopathy
The immediate cause of diabetic retinopathy is hyperglycemia( high blood sugar in the ). It leads to destructive changes in the walls of blood vessels.The first and main impact takes on the endothelium - the inner shell of the vessels.
Factors contributing to the vascular injury of the mesh membrane in diabetes mellitus:
-
 increased blood pressure, especially in those with "experience";
increased blood pressure, especially in those with "experience"; - smoking( even when smoking 1 cigarette a day, but regularly);
- kidney disease;
- pregnancy( regardless of the period);
- age, starting from 40 years.In the last 7-10 years, the risk of getting sick with retinopathy has spread to a young age - there are cases of the disease at the age of 20 years.Statistics of the lesion of young people are slowly but steadily increasing - this can lead to the fact that the age risk factor clinicians will establish, starting at the age of 25 years.
The hereditary peculiarity of the structure of the vascular wall plays an important role in the onset of diabetic retinopathy. If someone has suffered in one of the generations - the chances of getting sick from offspring are two or more times higher than those who first became ill on diabetes mellitus.
The most dangerous combination of factors leading to diabetic retinopathy is simultaneously observed hyperglycemia and high blood pressure.
Pathogenesis
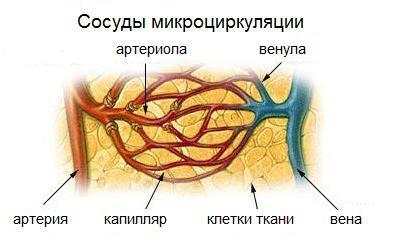
The pathogenesis( development) of diabetic retinal vascular injury is complex.It is based on a violation of microcirculation, that is, flaws in the "cooperation" of the smallest vessels and tissues to which blood vessels supply oxygen and nutrients to the blood stream.As a consequence, metabolic( metabolic) shifts occur in the cells of the retina.
The following structures of the mesh shell are mainly affected:
- arterioles( small arteries that are not anatomically yet capillaries) - they are most often deformed due to sclerosis( excessive formation of connective tissue);Most often they are affected by their precapillary segments in the posterior part of the fundus;
- veins - their expansion and deformation( curvature) are observed;
- capillaries - most often observed their dilatation( expansion, "blending" of one of the local areas), significantly increases permeability.In diabetic retinal lesions, capillaries are capable of swelling, this can lead to complete blockage and termination of inflow-outflow of blood along them with all the resulting metabolic consequences.Also, with diabetic retinopathy, the retinal capillaries manifestly suffer from endothelial overgrowth and the formation of microscopic aneurysms.
"Sweet" blood acts in two ways on the vessel wall - it can: become detached and deformed,
- ;
- thicken and deform.
In both cases, morphological changes lead to a disruption of the blood flow.This, in turn, entails:
- oxygen starvation of the tissues of the retina of the eye;
- violation of the intake of proteins, fats, carbohydrates, minerals in tissues;
- disruption of the output of vital activity from cells.
Hyperglycemia also causes to be hit on the hemato-retinal barrier.It consists of:
- endothelium( cells lining the inside of the retina vessels);
- of the pigment epithelium of the retina of the eye.
 Normally, the hemato-retinal barrier does not allow too large molecules to enter from the blood vessels into the tissues of the retina, thus protecting the retina from their destructive effects. When endothelial cells are affected in diabetes mellitus, their rows are thinning, the hemato-retinal barrier becomes more perceptive and is no longer able to withstand the onset of large molecules, which is fraught with retinal vital activity.
Normally, the hemato-retinal barrier does not allow too large molecules to enter from the blood vessels into the tissues of the retina, thus protecting the retina from their destructive effects. When endothelial cells are affected in diabetes mellitus, their rows are thinning, the hemato-retinal barrier becomes more perceptive and is no longer able to withstand the onset of large molecules, which is fraught with retinal vital activity.
The mesh of the eye is formed by the nerve cells .All nerve structures are characterized by increased sensitivity to negative factors and can not be restored. That's why if the process of their destructive changes is started due to starvation, it can not be turned back - except to stop, in order to save the remaining vital cells.This clearly explains the risk of diabetic retinopathy - you can prevent diabetic eye damage at some stage, but you can not resume lost vision. It should also be borne in mind that the retina consumes more oxygen per unit of area than other tissues of the human body.Therefore, even a minimal but constant oxygen starvation for it can be critical: the ischemia zones very quickly necrosis, the so-called cotton-like areas develop - local foci of the retinal infarction.

In diabetes mellitus, the vessels are affected not only by the retina of the eye.But diabetic retinopathy is the most common of all diabetic lesions of small vessels( microangiopathies).
The general scheme for the development of pathological changes in diabetic retinopathy is as follows:
- because of the complicated blood flow through the modified vessels of the retina, they at first dilatation( expansion), which leads to a short-term compensatory increase in blood flow;
- , while the endothelium is even more influenced by elevated blood sugar;
- capillaries swell more and more;
- , due to blood flow disorders on the capillaries, the blood is looking for new ways of progressing - as a result, arteriovenous shunts are formed( pathological connections between arterioles and venules that directly drain blood) and aneurysmal dilations of small vessels.Begins neovascularization - atypical germination of the retina with new vessels;
- new vessels, like affected "brethren," do not differ in strength, degenerative changes in their walls lead to their destruction and hemorrhages;
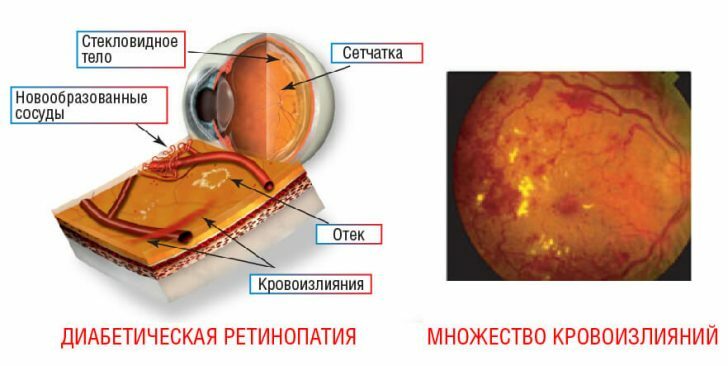
- as a result of such changes, focal changes occur in the retina of the eye, if they are massive - the retina degenerates completely, blindness occurs.
Classification
Ophthalmologists are guided by several classifications of diabetic retinopathies.
The most common classification is that proposed in 1992 by the doctors of Kohner E. and Porta M. and adopted by the World Health Organization.According to it, three forms of the disease are distinguished:
- non-proliferative retinopathy( diabetic retinopathy I);
- Pre-proliferative retinopathy( diabetic retinopathy II);
- proliferative retinopathy( diabetic retinopathy III).
 With of non-proliferative retinopathy, in the retina, the forming and already formed vascular microaneurysms are seen in the retina.Foci of hemorrhages are observed - first in the form of points that grow to round spots( sometimes bleeding in the form of strokes and short dots).They are of a dark color, they are defined in the central part of the fundus, and when examining the deep zones of the retina, larger ones along the veins.Also foci of exudate( sweating, or in simple words - moisture) are revealed closer to the center of the mesh shell, white and yellow, partly with clear, partially - with blurred boundaries. Important point: with non-proliferative retinopathy, retinal edema is always observed, if not, this is another form of diabetic retinopathy. Puffiness should be sought in the central part of the mesh shell or near large veins.
With of non-proliferative retinopathy, in the retina, the forming and already formed vascular microaneurysms are seen in the retina.Foci of hemorrhages are observed - first in the form of points that grow to round spots( sometimes bleeding in the form of strokes and short dots).They are of a dark color, they are defined in the central part of the fundus, and when examining the deep zones of the retina, larger ones along the veins.Also foci of exudate( sweating, or in simple words - moisture) are revealed closer to the center of the mesh shell, white and yellow, partly with clear, partially - with blurred boundaries. Important point: with non-proliferative retinopathy, retinal edema is always observed, if not, this is another form of diabetic retinopathy. Puffiness should be sought in the central part of the mesh shell or near large veins.
With , the pre-proliferative retinopathy shows changes in the retinal veins.They are like beads( like strung large beads on a string), are crooked, in some places - in the form of loops.If, in norm, the diameter of the veins was more or less the same, then with pre-proliferative retinopathy, it significantly fluctuates.There are observed "wadded"( similar to balls of cotton wool, unevenly "fluffy") exudates.There is also a large number of retinal hemorrhages.
With , proliferative retinopathy of , changes are observed not only in the retina, but beyond.Fragments of the retina sprout with new vessels - in the first place this process affects the visual disk.Throughout the volume of the vitreous body, a number of diffuse hemorrhages are determined - both pointlike, which merge with each other and form peculiar conglomerates.After a while, in places of hemorrhage, a fibrous tissue is formed, replacing the parts of the vitreous. Hemorrhage is a poor prognostic sign: after primary may occur secondary, which will lead to detachment of the weakened retina and blindness. Another serious complication is rubeosis( germination by the vessels of the iris) - a direct way to the emergence of secondary glaucoma.
A classification is also used that takes into account the morphological manifestations of the stages of diabetic angiopathy.It is described in the National Guidelines for Eye Disease.According to her, two forms are distinguished in diabetic retinopathy:
- pre-proliferative;
- is proliferative.
In turn, the following phases are distinguished in the preprofile form:
-
 vascular - with increasing changes in the wall of the vessels of the retina;
vascular - with increasing changes in the wall of the vessels of the retina; - exudative - with the appearance of a kind of condensate in the retina;
- hemorrhagic - with developing hemorrhages;In a number of cases, exudate( condensate) appears simultaneously and hemorrhages develop, then the phase is defined as exudative-hemorrhagic.
In the National Eye Disease Guide , the proliferative form is characterized by the following forms:
- with tissue vascularization( neovascularization);
- with gliosis;
- with partial or complete detachment of the mesh shell.
Gliosis is an increased amount of glia, which consists of cells that fill the space between neurons. In diabetic retinopathy, according to the classification, 4 degrees are distinguished:
- for grade 1 gliosis, glial cells are observed in the posterior fragment of the retina or in its middle section in the region of vascular arches( arches), but do not capture the optic nerve disk;
- Gliosis 2 degrees extends to the optic disc;
- with Gliosis 3 degrees of glia equally spreads both to the disk of the optic nerve, and to the vascular arcades;
- Gliosis 4 degrees - the most dangerous, with it the glia in the form of circular strips extends to the disk of the optic nerve, arches( arcades) of vessels and areas between arcades.
The clinical classification grades diabetic retinopathy into 4 varieties of :
- focal edematous - Ophthalmic examination of the mesh membrane determines edema spots;
- diffuse edematous - edema spreads all over the mesh membrane;
- ischemic - initially changes in the retinal vessels that lead to its oxygen starvation predominate;
- mixed - at the same time, swelling of the tissues of the mesh shell, and ischemic changes are observed.
Symptoms of diabetic retinopathy
At the initial stages of diabetic retinopathy, there are no clinical symptoms - the patient is not disturbed not by visual acuity, pain, or visual distortion. If a patient with diabetes complains that he has become poorly seen - this means that the pathological process in the tissues of the retina has gone far, moreover, it is irreversible.
The clinical manifestations of diabetic retinopathy are as follows:
-
 flashing "flies" before the eyes and spots that you unconsciously want to get rid of by blinking or wiping your eyes;The patient sees them because the vitreous body accumulates blood clots, formed due to destructive changes in the mesh shell;They are more clearly seen if you look at the light source;
flashing "flies" before the eyes and spots that you unconsciously want to get rid of by blinking or wiping your eyes;The patient sees them because the vitreous body accumulates blood clots, formed due to destructive changes in the mesh shell;They are more clearly seen if you look at the light source; - difficulty in working with texts( reading, writing) at close range - this indicates the development of swelling of the reticular membrane, in particular, its central fragment - the macula, which is responsible for visual acuity;
- 0emem can "compact";
- gradual reduction of visual acuity;
- partial loss of visual possibilities;
- complete loss of vision.
If a patient with diabetes has a "sight" and a veil before your eyes, you should contact the ophthalmologist in urgent order for help, otherwise you can suddenly lose your eyesight.
Since the clinical symptoms of diabetic retinopathy are delayed, instrumental methods for examining the retina are important for timely diagnosis: First of all, the following test methods are applicable: If the patient has intraocular pressure within normal limits, then methods that require medical dilatation of the pupils can be used for the study: The last two methods are considered to be the most sensitive and informative in detecting changes in retinal vessels caused by diabetic retinopathy. The ophthalmologist examines not only the retina, but other parts of the eyeball for differential( distinctive) diagnosis, since "flies", a veil before the eyes, visual acuity reduction is inherent in other ophthalmologic diseases( and not only ophthalmologic). The appointments are conducted jointly by the endocrinologist and oculist. The most important thing in the treatment of diabetic retinopathy is the appointment directed against diabetes mellitus - first of all, regulation of blood sugar level. If the newest methods were used to treat nosology, but blood sugar is not regulated - all performed manipulations will lead to a positive effect for a very short time. Therapeutic diet is important.Its main rules: Laser photocoagulation is a local, "point" cauterization of the affected sections of the mesh shell, which is performed to stop the pathological proliferation of blood vessels.It is performed on a laser coagulator.The principle of the procedure is simple: in the cauterized blood vessels the blood is clotted, the process of their deformation, causing the edema and detachment of the retina, the "excess" vessels that have already formed, are overgrown with a connective tissue. This is one of the most effective treatments for diabetic retinopathy. If it is performed on time, then it is possible to suspend the destruction of the retina: Even if this method is applied in the late stages of pathology development, vision can still be maintained in 55-60% of patients for 9-13 years.Sometimes in such patients, immediately after manipulation, visual acuity deteriorates - in particular, night vision deteriorates.But these are digestible results in comparison with the fact that the germination of the retina will be stopped by new vessels that act on it destructively. If diabetic retinopathy has a vitreous hemorrhage, is performed vitrectomy.This is an operation that is performed under anesthesia. It is prescribed in the following cases: The following medicines are also used: Preventive measures by which doctors can prevent diabetic retinopathy are all those methods that are aimed at the competent treatment of diabetes mellitus, stabilization of its course and transfer to a controlled channel.These are: Even if all these requirements are met with extreme punctuality, the subjective state of the patient satisfies him and the attending physician, and there is not the slightest change in sight - the should be examined with an ocular regularity with an enviable regularity. But not superficial, at the level of conversation, but complete, using all possible instrumental methods of diagnosis. Because of the delicacy of the retina, diabetic retinopathy can develop very quickly and just as quickly lead to irreversible changes in the structures of the eyeball - primarily the retina and the vitreous. If diabetic retinopathy is detected at the earliest stages, vision can be saved. Since blood sugar acts destructively on the walls of the retinal vessels, vision will gradually deteriorate over time even with ideally prescribed treatments - but these impairments are not catastrophic. Patients who strictly adhere to the correct medical appointments, adhering to a healthy lifestyle, regularly visit a competent ophthalmologist, blindness does not threaten. Kovtonyuk Oksana Vladimirovna, medical reviewer, surgeon, consulting physician
 biomicroscopic examination of the lens, as well as the vitreous( performed using a slit lamp);
biomicroscopic examination of the lens, as well as the vitreous( performed using a slit lamp); Treatment of diabetic retinopathy, principled approaches and methods
 Diabetic retinopathy requires serious interventions - in particular, invasive( with the introduction of an eyeball in the tissue). Despite the high degree of malignancy of the processes underlying diabetic retinopathy, 80% of cases of intervention can save a patient from blindness by applying invasive treatment techniques.
Diabetic retinopathy requires serious interventions - in particular, invasive( with the introduction of an eyeball in the tissue). Despite the high degree of malignancy of the processes underlying diabetic retinopathy, 80% of cases of intervention can save a patient from blindness by applying invasive treatment techniques.
 clots formed as a result of vitreous hemorrhage, do not resolve for more than six months;
clots formed as a result of vitreous hemorrhage, do not resolve for more than six months;
Prevention
Forecast