Postmenopausal osteoporosis: causes, symptoms, treatment
Osteoporosis that occurs in the postmenopausal period is an extremely important and socially significant problem of the modern world. Before proceeding to an analysis of the basic principles of therapy for this disease, it is necessary to carefully analyze some questions.
Content
- What is postmenopausal osteoporosis?
- Causes
- What factors predispose to postmenopausal osteoporosis?
- Detailed Mechanism of Menopausal Osteoporosis
- What Symptoms Indicate Postmenopausal Osteoporosis?
- How is the diagnosis carried out?
- What drugs are used for treatment?
- Bisphosphonates as the main link in the treatment of menopausal osteoporosis
- Nitrogen-containing
- Nitrogen-free
- Rules for taking bisphosphonate drugs
- Complications and side effects of bisphosphonate drugs
- Ways to Prevent Menopausal Osteoporosis
What is postmenopausal osteoporosis?
Postmenopausal osteoporosis Is a chronically progressive systemic metabolic disease of the skeleton due to a decrease in the content of minerals in human bone tissue, against the background of age-related extinction of ovarian function.
This defeat is very insidious, since outwardly it practically does not manifest itself in any way. Only in the later stages can a woman be bothered by pain in the joints, back, until everything develops into frequent fractures.
In the first 5 years after menopause, the skeletal system loses almost a third of its mineral components, and taking into account increase in the general age of the population, the problem of menopausal osteoporosis is becoming more and more relevant.
Causes
The main reasons for the development of the disease are considered to be:
- Decreased levels of female hormones estrogen. One of the functions of the hormone estrogen is to participate in the regulation of mineral metabolism, including calcium metabolism, which is the main element of the human musculoskeletal system. After the extinction of the reproductive function, the level of estrogen in the body decreases, which means that the level of the main component of the skeletal system decreases. As a result, it becomes porous, soft, and ceases to withstand loads. This is called menopausal osteoporosis..
- Poor nutrition. Another factor, the importance of which is often underestimated. Experts note that most of those suffering from this pathology follow an extremely inadequate diet. Such people, as a rule, do not consume enough dairy products, meat, herbs, beans, vegetables. In addition, they do not compensate for this deficiency in any way, which inevitably leads to a calcium deficiency in the body.
- Low level of mobility. With age, the physical activity of most people, including women, decreases markedly. There can be many reasons: heavy somatic diseases, excess weight, the consequences of injuries and emergencies in the past. All this also leads to less time spent outdoors, which entails a decrease in production in the body. vitamin Dwhich is an essential component for the successful absorption of calcium and the maintenance of bone density.
What factors predispose to postmenopausal osteoporosis?
Risk groups include persons:
- over 65;
- who have menopause early;
- smoking abusers;
- alcohol abusers;
- having hormonal disorders, especially disorders of hormones of the thyroid gland, adrenal glands, pituitary gland;
- with a genetic predisposition.
Detailed Mechanism of Menopausal Osteoporosis
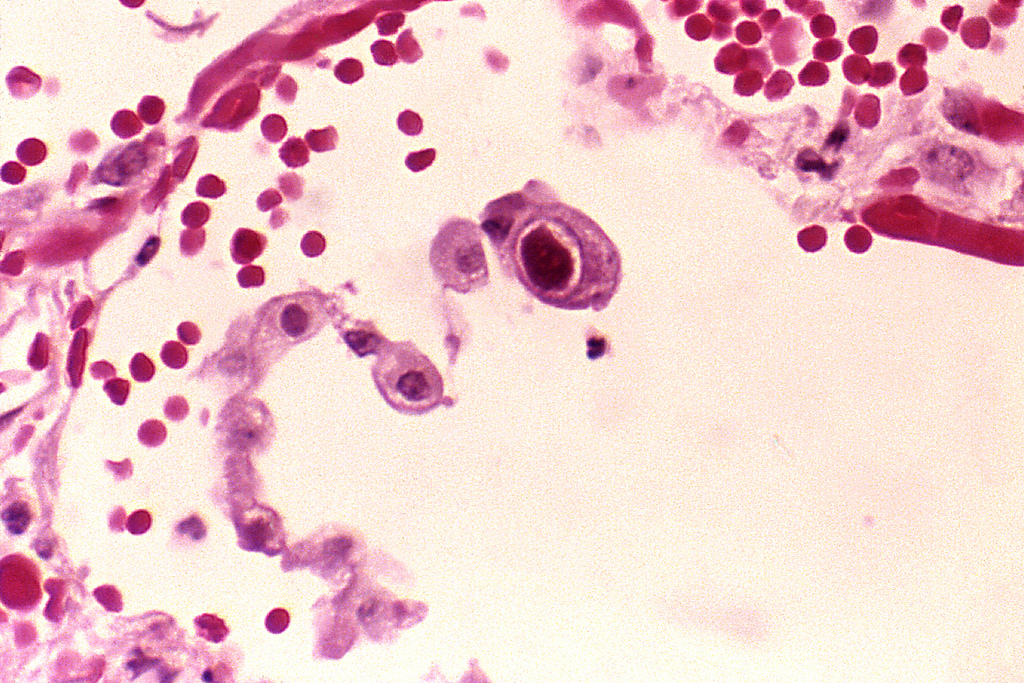
In the bone tissue of a healthy person, the processes of remodeling, that is, restructuring, are constantly taking place. Cells continuously re-form and resorb bone. This balance is maintained by a number of hormones that are closely related to each other.
Read also:Ovarian cyst cystectomy: surgical removal method
After the end of the period of functioning of the reproductive function of a woman, the ovaries cease to perform their tasks, including the production of sex hormones, in particular estrogen. The synthesis of estrogen is associated with the synthesis of calcitonin, which, in turn, lowers the level of parathyroid hormone.
Parathyroid hormone increases the content of calcium ions in the blood due to increased absorption in the intestine, due to resorption of bone tissue and a decrease in its excretion in the urine.
As mentioned above, inadequate nutrition and inadequate physical activity lead to a deficiency in the intake of calcium in the body. Therefore, the only result will be permanent bone destruction.
Additional causes are vitamin D deficiency, which is directly involved in calcium absorption; insufficient bowel function due to inevitable aging processes, which is the reason for insufficient absorption of calcium from food; low mobility that disrupts an adequate blood supply to the bones.
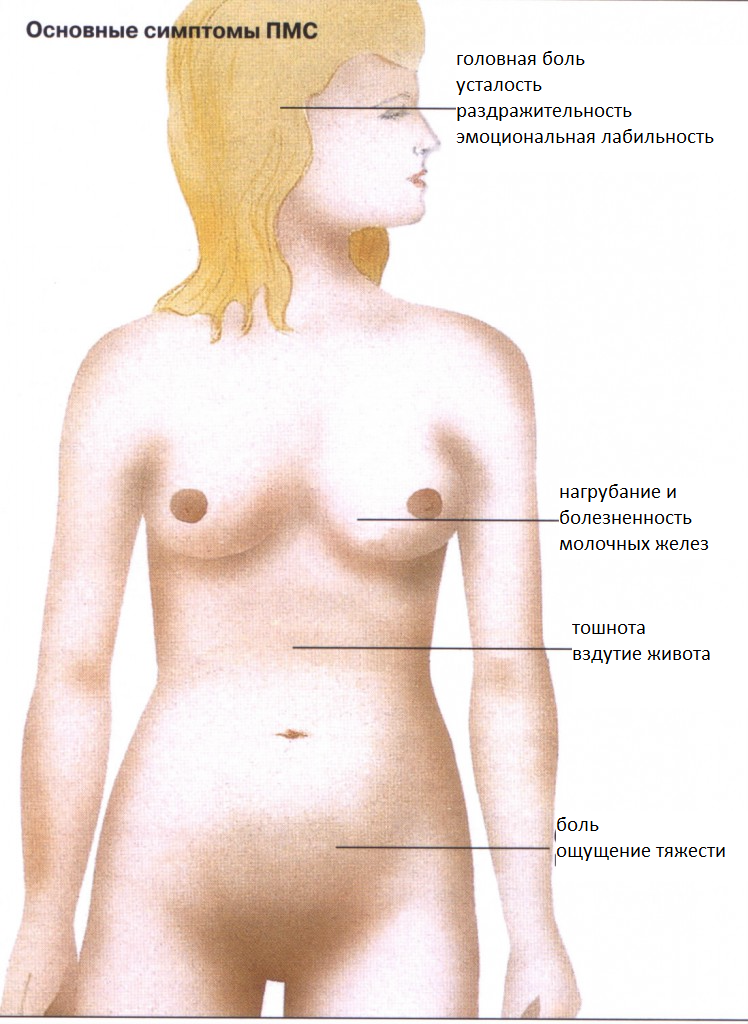
What Symptoms Indicate Postmenopausal Osteoporosis?

Unfortunately, due to its asymptomatic nature, menopausal osteoporosis cannot be diagnosed on its own. As a rule, such a diagnosis is made in a hospital after a woman is admitted there with a spontaneous fracture.
The primary signs that are usually ignored are - back pain, back, pelvis, legs, jointsthat appears after physical exertion and disappears after rest, increased fatigue, night cramps leg muscles. Over time, these symptoms bother the woman more and more.
It can also alert curvature of the spine in the form of a "hump", a decrease in height by several centimeters per year, a decrease in body weight without changing volumes and proportions.
Late referral to a specialist leads to spontaneous fractures of the femoral neck, forearms, lower legs, and thoracic spine. All this together can lead to severe disability of a person and impairment of his mental health.
How is the diagnosis carried out?

After taking a history and identifying risk factors for menopausal osteoporosis, the specialist prescribes studies designed to assess the condition of bone tissue, as well as detect signs of it in blood tests destruction.
The most common methods are:
- Densitometry. It is carried out with the help of an apparatus, the action of which is based on X-ray radiation. It evaluates bone density. The same study is available using ultrasound diagnostics, as well as using computed tomography. Areas of the skeleton most susceptible to osteoporosis: spine, hip joint, pelvic bones, humerus, radius, hands, feet.
- Blood chemistry. Here, attention is paid to the amount of calcium, phosphorus, alkaline phosphatase, osteocalcin, which are direct evidence of bone destruction. In some cases, they additionally carry out Analysis of urine for calcium content.
- Blood test for hormone levels. First of all, the level of thyrocalcitonin and parathyrin, thyroid hormones responsible for the balance of calcium in the body, is determined. An additional study of the content of sex hormones makes it possible to make a definitive diagnosis of menopausal osteoporosis.
Read also:Aerobic vaginitis
What drugs are used for treatment?
Modern methods of therapy for postmenopausal osteoporosis are aimed at eliminating the links of the pathological process. Medicines increase bone mineralization, suspend resorption processes and prevent complications.
Main groups:
- Bone formation stimulants. This group includes hormonal and steroid drugs, minerals. They act on the hormonal regulation of bone destruction and stimulate cells to form new tissue.
- Preparations with multidimensional action. These include, first of all, calcium preparations in combination with vitamin D. This combination promotes adequate absorption of the mineral, which allows the body to successfully use it to build new bone tissue. Flavone compounds and ossein-hydroxylate complexes inhibit the processes of skeletal destruction, inhibiting the activity of the cells responsible for this.
- Medicines that prevent bone resorption mechanisms. In addition to hormonal drugs, this group includes bisphosphanates. It also includes hormonal agents: estrogens and progestins, calcitonin.
Bisphosphonates as the main link in the treatment of menopausal osteoporosis

To put it simply, the mechanism of bisphosphonate preparations is to suppress the functions of osteoblasts, cells that destroy bone tissue. That is, they act on the final link of osteoporosis.
These medicines have been used for a long time, since the middle of the twentieth century. Since then, many new drugs have been invented that can be divided into three generations.
The use of bisphosphonates has become possible in the treatment of oncological diseases, since they are able to prevent tumor metastasis.
All drugs based on bisphosphonates can be divided into two large groups:
- nitrogen-free
- nitrogen-containing
Due to their molecular structure, they have peculiarities in the mechanism of action, which determines the area of their application in the treatment of menopausal osteoporosis.
Nitrogen-containing
Bisphosphonate preparations belonging to this group contain a number of active substances that determine their properties, pharmacodynamics and pharmacokinetics:
- Alendronate sodium is the basis for second generation drugs. It is a specific regulator of bone metabolism, which has a non-hormonal nature. Therefore, bisphosphonate preparations with this active substance can be used in both men and women.
- Ibandronic acid (INN) or sodium ibandronate is the basis of a number of third generation drugs. It is indicated for women who have entered a complicated menopausal phase, for the prevention of osteoporosis, as well as in the case of a pathologically high content of calcium ions in the blood. The use of bisphosphonates from this group is not recommended for men.
- Zoledronic acid. Its unique property lies in its molecular relationship with the structure of bone tissue, which determines the selective action of these drugs. Studies have found that bisphosphonate preparations containing zoledronic acid also have anticancer effects.
Nitrogen-free
Representatives of this group belong to the first generation. But do not think that these are outdated and ineffective drugs. The use of nitrogen-free bisphosphonates is still widespread in the treatment of menopausal osteoporosis.
- Sodium tiludronate. It is widely used in the treatment of patients with deforming osteodystrophy and Paget's disease. Slows down the destruction of bone tissue, promotes the accumulation of calcium and phosphates in it, increasing the percentage of minerals.
- Sodium etidronate. It is prescribed for Paget's disease, osteoporosis, an increase in calcium ions in the blood.
- Clodronate. Affects the final links of menopausal osteoporosis: inhibits the process of resorption of bone tissue and prevents the leaching of calcium from it. This compound is able to integrate into the structure of the skeleton, changing its chemical composition, strengthening the bonds between molecules.
Read also:Anovulation: what is it, causes, symptoms and treatment of this disease
Rules for taking bisphosphonate drugs
These medicinal substances are classified as potent groups, and therefore their purpose, dose and mode of administration should be strictly controlled by a doctor. In order for the selected therapy to be as effective as possible and not cause side effects, it is necessary to adhere to the following rules for the use of bisphosphonates:
- the drug should be taken on an empty stomach, half an hour before breakfast;
- drink pills with plenty of clean water;
- do not take a horizontal position for an hour;
- preparations containing calcium in combination with vitamin D should be consumed 2-3 hours after the use of bisphosphonates.
Complications and side effects of bisphosphonate drugs
Any serious illness requires effective and potent medicines. Despite the high efficiency, the use of bisphosphonates is often accompanied by a number of undesirable manifestations and the occurrence of pathological conditions:
- damage to kidney tissue;
- hypocalcemia, that is, a condition in which there are too few calcium ions in the blood;
- ulcerative lesions of the gastrointestinal tract;
- digestive disorders;
- disorders of the heart;
- increased risk of developing osteonecrosis as a result of trauma, including in the jaw area after tooth extraction and treatment;
- allergic reactions;
- skin reactions;
- muscle pain, general malaise, joint aches, fever;
- visual impairment.
Ways to Prevent Menopausal Osteoporosis

No matter how trite it may sound, it is much easier and cheaper to prevent the development of some pathological condition than to treat it. The main conditions for reducing the risk of developing osteoporosis:
- Maintaining a healthy lifestyle. Quitting smoking and alcohol will largely contribute to the long-term preservation of the functions of all organ systems.
- The optimal mode of physical activity. Physical inactivity causes the development of degenerative processes in the musculoskeletal system, including bone tissue.
- Balanced diet. Every day with food, the body must receive all the necessary minerals and trace elements. Diets based on reducing the proportion of fat consumed can also contribute to the development of osteoporosis later in life.