Angioedema: what is it, symptoms, photos, treatment
Content
- What is angioedema?
- How does angioedema differ from urticaria?
- Causes
- Symptoms (photo)
- Diagnostics
- Treatment and prevention
What is angioedema?
Angioedema (synonyms: angioedema, angioedema, angioedema, Quincke's edema) Is an inflammatory skin response similar to hives, characterized by the sudden appearance of edema in areas of the skin, mucous membranes and submucosal membranes. Symptoms of angioedema can affect any part of the body, but most often affect the eyes, lips, tongue, throat, genitals, arms and legs.
Angioedema, in more severe cases, also affects the lining of the airways and the upper intestine, causing chest or abdominal pain. Angioedema is short-lived: usually swelling in the affected area lasts from one to three days.
In most cases, the reaction is harmless and leaves no trace, even without treatment. The only danger is that this can hurt the throat or tongue, as their severe swelling can cause rapid airway obstruction. shortness of breath and loss of consciousness.
How does angioedema differ from urticaria?

Angioedema and urticaria are the result of the same pathological process, so in some respects they are similar:
- Often, both clinical manifestations coexist and overlap: urticaria is accompanied by angioedema in 40-85% of cases, while angioedema can occur without urticaria in only 10% cases.
- Urticaria is less severe because it affects only the surface layers of the skin. Angioedema, on the other hand, affects deep subcutaneous tissue.
- Urticaria is characterized by the temporary onset of an erythematous and itchy reaction in well-defined areas of the dermis (the appearance of more or less red and raised blisters). With angioedema, on the other hand, the skin retains its normal appearance without blisters. In addition, the swelling can occur without itching.
The main differences between urticaria and angioedema are shown in the following table:
| Peculiarity | Angioedema | Hives |
| Involved tissue | Hypodermis (subcutaneous layer) and submucosa (below the dermis). | Epidermis (outer layer of skin) and dermis (inner layer of skin). |
| Affected organs | Skin and mucous membranes, in particular the eyelids, lips and oropharynx. | Only leather. |
| Duration | Transient (24-96 hours). | Transient (usually <24 hours). |
| Physical signs | Swelling (swelling) under the surface of the skin. | Erythematous and blistering patches on the surface of the skin. |
| Symptoms | Itching may or may not be present. Angioedema is often accompanied by pain and swelling. | The rash associated with hives is usually itchy. Pain and swelling are not common symptoms. |
Causes
Depending on the causes of angioedema, it can be classified in different forms: acute allergic, medicinal (non-allergic), idiopathic (spontaneous), hereditary and acquired.
| Type of angioedema and clinical features | Causes |
|
Allergic angioedema. The swelling is caused by an acute allergic reaction, almost always associated with hives, which occurs within 1–2 hours of exposure to the allergen. Sometimes this is accompanied by anaphylaxis. Reactions are self-limiting and resolve within 1–3 days, but may recur with repeated exposures or due to interactions with cross-reactive substances. |
|
|
Non-allergic drug reaction. Some medicines can cause angioedema as a side effect. Onset may occur several days or months after the first dose of the drug due to a cascade of effects, which cause the activation of the quinine-kallikrein system, the metabolism of arachidonic acid and the formation of oxide nitrogen. |
Less common causes of drug-induced angioedema include taking:
|
|
Idiopathic angioedema. In some cases, there is no known cause of angioedema, although some factors can cause symptoms. The idiopathic form is often chronic and recurrent and usually occurs with urticaria. In some people, when the condition occurs for years without an obvious cause, an autoimmune process may exist at the base. |
|
|
Hereditary angioedema. Autosomal dominant hereditary disease. Hereditary angioedema is characterized by low serine protease inhibitor (inhibitor C1 or C1-INH), which helps maintain the stability of blood vessels and regulates the flow of fluid into fabrics. Decreased C1 inhibitor activity results in excess kallikrein, which in turn produces bradykinin, a potent vasodilator. |
|
|
Acquired angioedema. Acquired C1 inhibitor deficiency. |
|
Regardless of the cause of angioedema, the main pathological process is the same in all cases: edema is the result of loss of fluid from the walls of small blood vessels that supply the subcutaneous fabrics.
Histamine and other inflammatory chemical mediators are released into the skin that cause redness, itching and swelling. Mast cells of the skin or mucous membrane are involved in various processes.
Mast cell degranulation * releases primary vasoactive mediators such as histamine, bradykinin and other kinins; secondary mediators such as leukotrienes and prostaglandins are subsequently released, which contribute to inflammatory reactions both early and late, with increased vascular permeability and fluid leakage into surface tissues.
Triggers and mechanisms involved in the release of these inflammatory mediators make it possible to identify different types of angioedema.
* Degranulation - release of biologically active substances (chemical mediators of allergy) from mast cells.
Symptoms (photo)

Clinical signs of angioedema may differ slightly between different forms, but in general, the following manifestations appear:
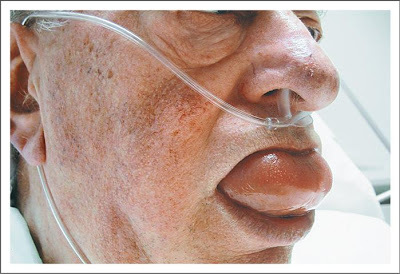
- Localized edema, usually affecting the periorbital region, lips, tongue, oropharynx, and genitals (see photo above);
- The skin may appear normal, that is, without hives or other rashes;
- Pain, fever, itching, tingling, or burning in the affected areas;
Other symptoms may include:
- Abdominal pain caused by swelling of the mucous membrane of the gastrointestinal tract, with nausea, vomiting, seizures and diarrhea;
- Swelling of the bladder or urethra, which can cause difficulty urinating;
- In severe cases, swelling of the throat and / or tongue can make it difficult to breathe and swallow. photo below).
Diagnostics
Diagnosis of angioedema is relatively simple. Due to its appearance, the physician should be able to recognize it after a simple physical examination and a detailed medical history.
Additional tests, such as a blood test, may be required to accurately determine the type of angioedema.
To detect allergens (allergic angioedema), allergy tests. Hereditary angioedema can be diagnosed with a blood test to check the level of proteins regulated by the C1-INH gene: a very low level confirms the presence of the disease.
The diagnosis and treatment of hereditary angioedema is highly specialized and should be performed by a clinical immunologist.
Angioedema can be associated with other medical problems such as iron deficiency, liver disease and the thyroid gland, which doctors will examine with simple blood tests (it is helpful to check or rule out these conditions).
Idiopathic angioedema is usually confirmed by what is known as a "rule out diagnosis"; in practice, the diagnosis is confirmed only after various studies have been carried out to exclude any other disease or condition with similar manifestations.
Treatment and prevention
Treatment of angioedema depends on the severity of the condition. In cases of airway involvement, the first priority is to ensure that the airways are open. Patients may require urgent inpatient treatment and intubation.
In many cases, the swelling is self-limited and goes away spontaneously after a few hours or days. In the meantime, to help alleviate milder symptoms, you can try these measures:
- Eliminate specific triggering factors;
- Take a cold shower (but not too long) or put a cold bag on the affected area;
- Wear loose clothing;
- Try not to rub or scratch the affected area;
- Take an antihistamine to relieve itching.
In severe cases, if swelling, itching, or pain persists, the following medications may be indicated:
- Oral or intravenous corticosteroids;
- Antihistamines by mouth or by injection;
- Epinephrine injections (epinephrine).
The goal of angioedema treatment is to reduce symptoms to an acceptable level and to ensure normal activities (such as work or night rest).
Angioedema associated with chronic autoimmune or idiopathic urticaria is often difficult to treat and drug response varies. In general, the following processing steps are recommended, where after each step the following is added if therapy does not provide an adequate response:
- Step 1: non-sedating antihistamines, such as Cetirizine;
- Step 2: sedative antihistamines, such as Diphenhydramine;
- Step 3:
- a) oral corticosteroids, for example Prednisone;
- b) immunosuppressants, for example Cyclosporine and Methotrexate.



