Vertebral artery syndrome: symptoms, treatment, prognosis
Content
- What is vertebral artery syndrome?
- Causes of the vertebral artery syndrome
- Symptoms of the vertebral artery syndrome
- Clinical types of the syndrome
- Posterior cervical sympathetic syndrome (Barre-Lieu)
- Basilar migraine
- Vestibulo-cochlear syndrome
- Ophthalmic Syndrome
- Autonomic change syndrome
- Transient (transient) ischemic attacks
- Syncope Vertebral Syndrome (Unterharnscheit Syndrome)
- Drop Attack Episodes
- Diagnostics
- Treatment of vertebral artery syndrome
- Drug treatment
- Neuroprotective therapy
- Forecast
- Prophylaxis
What is vertebral artery syndrome?
Vertebral artery syndrome (abbr. SPA or cervical migraine, Barre-Lieu syndrome, vertebral artery syndrome, posterior cervical sympathetic syndrome) Is a pathology that appears as a result of compression of the nerves surrounding the vertebral artery.
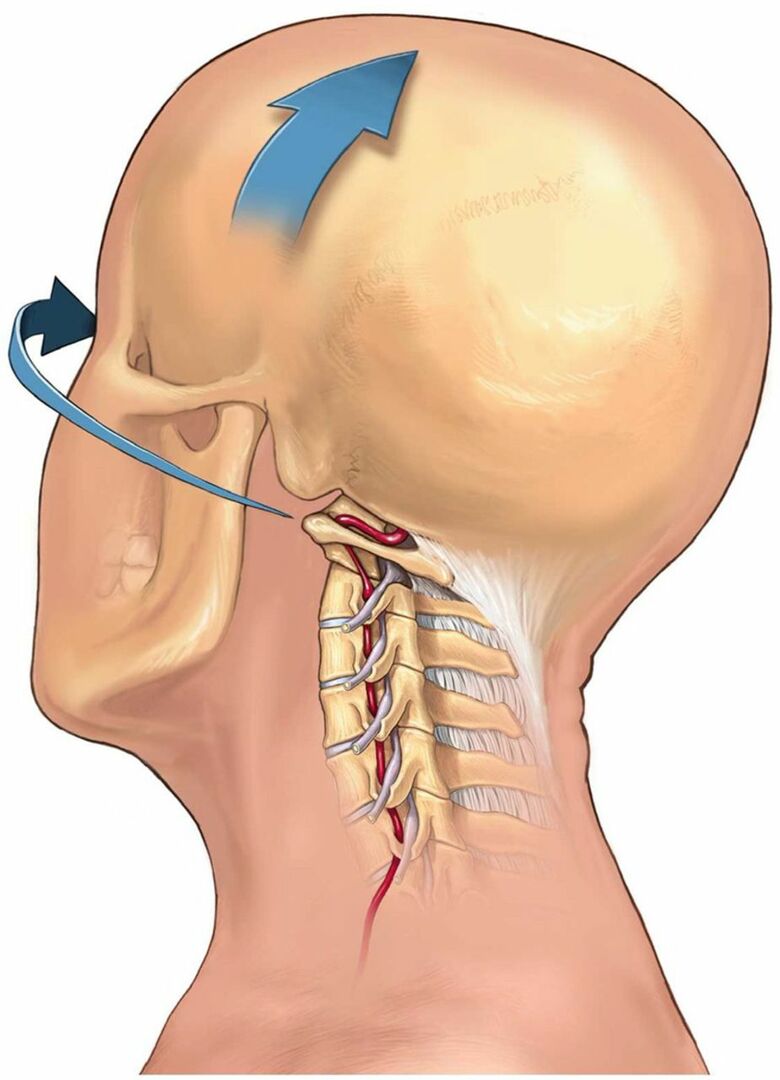
SPA occurs as a result of damage to the 1st, 2nd and 3rd cervical vertebrae, when the roots of the spinal nerves that braid the vertebral artery are compressed. The artery is also compressed. The result is circulatory failure, nervous edema and stagnation of venous blood.
Circulatory failure develops not only where the vertebrae have been damaged, but also in some areas of the brain.
Damage to the vertebrae can result from trauma, spinal tumors, osteochondrosis, spondylosis. Cervical lymphadenitis (inflammation of the lymph nodes in the neck), cervical arachnoiditis (inflammation of the arachnoid membrane of the spinal cord), or compression of the vertebral arteries.
During seizures, the sufferer is often disabled.
Causes of the vertebral artery syndrome
The main reasons for the development of vertebral artery syndrome are the following pathologies:
- Vascular diseases with impaired vascular patency, such as atherosclerosis, various arthritis, embolism.
- Changing the shape of the arteries (deformities) - abnormal tortuosity, significant kinks, abnormal structural changes in the arteries.
- Extravasal compression (compression) of vessels (compression of arteries by osteophytes, hernias, disc protrusions, bone anomalies, tumors, scar tissue)
Given that various factors can cause the syndrome, sometimes difficulties arise in interpreting the diagnosis, since this syndrome can denote a variety of conditions, for example, acute disorders blood circulation. But in clinical practice, degenerative-dystrophic changes in the cervical spine and abnormal phenomena with sides of the atlas, which lead to impaired blood flow in the basin of the vertebral arteries and the appearance of symptoms of cerebral impairment blood circulation.
Distinguish between extracranial and intracranial parts of the vertebral artery.
A significant part of the extracranial vertebral arteries pass through a movable canal formed by holes in the transverse processes of the vertebrae. The sympathetic nerve (Frank's nerve) also passes through this channel. At the C1-C2 level, the vertebral arteries are closed only by soft tissues. This anatomical feature of the passage of the vertebral arteries and the mobility of the cervical spine significantly increase the risk of developing a compression effect on the vessels from the surrounding tissues.
The resulting compression from the surrounding tissues leads to compression of the artery of the vegetative endings and vascular constriction due to reflex spasm, which leads to insufficient blood supply to the head brain.
Often the reasons for the compression of arteries and the development of SPA are:
- degenerative changes in the cervical spine:
- cervical osteochondrosis;
- arthrosis of the facet joints;
- uncovertebral arthrosis;
- instability of motor segments;
- herniated discs;
- deforming spondylosis of the cervical spine;
- bone growths (osteophytes);
- muscle reflex syndromes:
- inferior oblique muscle syndrome:
- anterior scalene muscle syndrome.
Read also:Polyneuropathy of the upper and lower extremities: causes, symptoms and treatment of pathology
Most often, compression occurs at the level of 5-6 vertebrae, a little less often at the level of 4-5 and 6-7 vertebrae.
The most common reason development of vertebral artery syndrome is uncovertebral syndrome. The proximity of these joints to the vertebral arteries leads to the fact that even small bone or osteochondral growths (exostoses) in the area of the uncovertebral joints lead to a mechanical effect on vertebral arteries. With significant uncovertebral exostoses, significant compression of the lumen of the vertebral arteries is possible.
Anomalies of Kimberley and Powers play a rather significant role in the development of the vertebral artery syndrome.
Symptoms of the vertebral artery syndrome

According to the clinical course, there are two stages of SPA:
- functional;
- organic.
The functional stage of the syndrome is characterized by a certain group of symptoms: headaches with some autonomic disturbances, cochleovestibular and visual disturbances. Headache can take many forms:
- acute pulsating;
- aching constant;
- sharply increasing, especially when turning the head or prolonged static load.
The headache can spread from the occiput to the forehead. Disorders in the cochleovestibular system may manifest as dizziness of a paroxysmal nature (unsteadiness of swinging) or systemic dizziness. In addition, there may be some hearing loss. Visual disturbances can be manifested by darkening in the eyes, a feeling of sparks, sand in the eyes.
Long and prolonged episodes of vascular disorders lead to the formation of persistent foci of ischemia in the brain and the development of the second (organic) stage of the vertebral artery syndrome.
In the organic stage of SPA, symptoms of both transient and persistent hemodynamic disorders of the brain appear. Transient hemodynamic disorders are manifested by symptoms such as:
- dizziness;
- nausea;
- vomit;
- dysarthria.
In addition, there are characteristic forms of ischemic attacks that occur during turning or tilting the head, in which they can there are seizures of falling with preserved consciousness, the so-called drop attacks, as well as seizures with loss of consciousness lasting up to 10 minutes (syncope episodes).
Symptoms tend to regress in the horizontal position and are thought to be due to transient ischemia of the brainstem. After such episodes, you may experience:
- general weakness;
- noise in the ears and head;
- vegetative disorders.
According to the type of hemodynamic disorders, several variants of the vertebral artery syndrome are distinguished (compression, irritative, angiospatic and mixed forms).
The narrowing of the vessel in the compression version occurs due to mechanical compression on the artery wall. In the irritative type, the syndrome develops as a result of reflex vasospasm due to irritation of sympathetic fibers. In the clinic, most often, there are combined (compression-irritative) variants of the vertebral artery syndrome.
With the angiospastic variant of the disease, there is also a reflex mechanism, but it arises from irritation of the receptors in the region of the motor segments of the cervical spine. With the angiospastic variant, vegetative-vascular disorders predominate and the symptomatology is not so strongly caused by head turns.
Clinical types of the syndrome
Posterior cervical sympathetic syndrome (Barre-Lieu)
The posterior cervical syndrome is characterized by headaches localized in the cervico-occipital region radiating to the front of the head. The headache is usually constant, often in the morning, especially after sleeping on an uncomfortable pillow. Headache may occur when walking, driving a car, or when moving in the neck.
Read also:ENMG examination (electroneuromyography) - what is it?
The headache can also be pulsating, piercing with localization in the cervico-occipital region and with irradiation to the parietal frontal and temporal zones. The pain can intensify when turning the head and is accompanied by both vestibular and visual and autonomic disorders.
Basilar migraine
Basilar migraine occurs not as a result of compression of the vertebral artery, but as a result of stenosis vertebral artery, but clinically has much in common with other forms of vertebral syndrome arteries.
As a rule, a migraine attack begins with a sharp headache in the occiput, vomiting, and sometimes with loss of consciousness. Visual disturbances, dizziness, dysarthria, ataxia are also possible.
Vestibulo-cochlear syndrome
Hearing system disorders are manifested in the form of noise in the head, a decrease in the perception of whisper speech and are recorded by changes in the data during audiometry. Tinnitus is persistent and long lasting and tends to change in character with head movement. Cochlear disorders are associated with vertigo (both systemic and non-systemic).
Ophthalmic Syndrome
In ophthalmic syndrome, visual disturbances such as atrial fibrillation are in the foreground, decreased vision, photopsy may also be conjunctivitis symptoms (lacrimation conjunctival hyperemia). The loss of visual fields can be episodic and are mainly associated with a change in the position of the head.
Autonomic change syndrome
As a rule, autonomic disorders do not appear in isolation, but are combined with one of the syndromes. Vegetative symptoms are typically as follows:
- feeling of heat;
- feeling of coldness of the limbs;
- sweating;
- changes in skin dermographism;
- sleep disorders.
Transient (transient) ischemic attacks
Transient ischemic attacks can occur during the ischemic stage of SPA. The most common symptoms of these attacks are:
- transient motor and sensory disorders;
- visual impairment;
- hemianopsia;
- ataxia;
- dizziness attacks;
- nausea;
- vomit;
- violation of speech, swallowing;
- double vision.
Syncope Vertebral Syndrome (Unterharnscheit Syndrome)
An episode of syncope vertebral syndrome is an acute circulatory disorder in the reticular formation of the brain. This episode is characterized by a short-term blackout with a sudden turn of the head.
Drop Attack Episodes
The episode of a drop attack (fall) is caused by impaired blood circulation in the caudal parts of the brain stem and the cerebellum and will clinically manifest as tetraplegia (paralysis of the four limbs) when rolling back heads. However, motor functions are restored fairly quickly.
Diagnostics
Diagnostics of the vertebral artery syndrome presents certain difficulties and often occurs both an erroneous medical opinion (overdiagnosis) and underdiagnosis (no diagnosis) SPA. Overdiagnosis of the syndrome is often due to insufficient examination of patients, especially in the presence of vestibulo-atactic and / or cochlear syndrome, when the doctor fails to diagnose the disease labyrinth.
To establish a diagnosis of vertebral artery syndrome, 3 criteria are required.
- The presence of symptoms in the clinic of one of 9 clinical options or a combination of options
- Visualization of morphological changes in the cervical spine using magnetic resonance imaging (MRI) or multislice computed tomography (MSCT), which may be the main causes of this syndrome.
- The presence of changes in blood flow during ultrasound examination (ultrasound) during functional tests with flexion - extension of the head by rotating the head.
Read also:Kearns-Sayre Syndrome
Treatment vertebral artery syndrome
Treatment of vertebral artery syndrome (SPA) consists of two main areas:
- improved hemodynamics;
- treatment of diseases leading to compression of the vertebral arteries.
Drug treatment

Anti-inflammatory and decongestant therapy is aimed at reducing perivascular edema resulting from mechanical compression. Prescribe drugs that regulate venous outflow:
- troxerutin
- ginkgo biloba
- diosmin.
Non-steroidal anti-inflammatory drugs (NSAIDs):
- celebrex;
- lornoxicam;
- celecoxib.
Vascular therapy is aimed at improving blood circulation in the brain, since hemodynamic disorders occur in 100% of patients with SPA. Modern diagnostic methods make it possible to evaluate the effectiveness of treatment with these drugs and the dynamics of blood flow in the vessels of the brain using ultrasound studies.
The following drugs are used for vascular therapy:
- purine derivatives (trental);
- vinca derivatives (vincamine, vinpocetine);
- calcium antagonists (nimodipine);
- alpha-blockers (nicergoline, sermion).
Neuroprotective therapy
One of the most modern areas of drug treatment is the use of drugs to improve energy processes in the brain, which minimizes damage to neurons due to episodic disorders blood circulation. Neuroprotective agents include:
- cholinergic drugs (citicoline, gliatilin);
- drugs that improve regeneration (Actovegin, Cerebrolysin);
- noootropes (piracetam, mexidol);
- metabolic drugs (mildronate, thiotriazoline, trimetazidine).
Symptomatic therapy includes the use of drugs such as:
- muscle relaxants;
- anti-migraine drugs;
- antihistamines and others.
Treatments for degenerative diseases include non-drug treatments such as:
- Exercise therapy (remedial physical culture);
- physiotherapy;
- massage;
- acupuncture;
- manual therapy.
In most cases, the use of complex treatment, including both drug and non-drug treatment, can reduce symptoms and improve blood circulation in the brain.
Surgical treatments are used when there is severe compression of the arteries (disc herniation, osteophyte) and only surgical decompression can achieve clinical result.
Forecast
The prognosis for SPA depends on the current symptoms, health status and age of the patient. Young people who experience mild symptoms and control them through lifestyle changes and medication usually have good results. Old age, weakness and stroke can negatively affect the forecast.
Prophylaxis
To reduce the risk of developing vertebral artery syndrome, it is recommended to resort to a number of actions:
- perform exercises for the shoulder girdle and neck every hour if the work is associated with a prolonged sitting position;
- use an orthopedic mattress and pillow for day and night rest;
- avoid throwing your head back during sleep;
- refrain from excessive consumption of strong alcoholic beverages;
- every year take a course of massage of the collar zone;
- if possible, allow yourself to stay in sanatoriums whose work is aimed at preventing and treating neurological pathologies (especially if you are at risk).



