Carbon monoxide poisoning: causes, symptoms, treatment, complications
Content
- Introduction
- Causes and risk factors
- Symptoms
- Frequent symptoms
- Rare symptoms
- Complications and consequences
- When to see a doctor
- Diagnostics
- How is carbon monoxide poisoning treated?
- Traditional treatment
- Hyperbaric oxygen therapy
- Prophylaxis
Introduction
Carbon monoxide poisoning occurs when a person inhales too much carbon monoxide (CO, carbon monoxide), which is colorless, not odorless gas resulting from the combustion of fuel containing carbon - gasoline, diesel fuel, fuel oil, natural gas, coal, firewood.
Symptoms include headache, dizziness, weakness, vomiting, chest pain, and confusion. Excessive exposure to CO can lead to severe heartbeat disorders, seizures, loss of consciousness, and even death.
Carbon monoxide poisoning can be diagnosed with a CO oximeter, a non-invasive device that measures CO in the blood. Treatment usually involves supplying oxygen under pressure through a non-circulating mask. Severe cases may require treatment in a hyperbaric oxygen chamber.
Causes and risk factors
Carbon monoxide poisoning is caused by the inhalation of carbon monoxide (CO). The gas is colorless and odorless. It binds to hemoglobin, an iron-based protein in red blood cells, which gives them red color and carries oxygen. Only a small amount of carbon monoxide in the air is required to displace oxygen molecules from hemoglobin, and this amount is usually supplied randomly from various combustion sources.
Carbon monoxide is a natural by-product of combustion. In most cases, poisoning occurs when the gas is inhaled, as it quickly accumulates in an enclosed space (usually due to faulty ventilation).
Poor ventilation in a confined space leads to poisoning. Some cases of accidental carbon monoxide poisoning are due to the inappropriate use of devices such as stoves, gas appliances, or generators inside homes or buildings. However, most incidents are due to equipment failure, usually associated with ventilation problems in ovens or cars.
Common sources of CO include:
- wood stoves;
- home fires;
- vehicle exhaust;
- gas or propane stoves and grills;
- charcoal grills;
- non-ventilated propane, kerosene or gas heaters;
- gas electric generators;
- gas dryers for clothes.
Source of Carbon Monoxide (CO) The vast majority of all intentional carbon monoxide poisoning comes from cars or other internal combustion engines.
Symptoms

Carbon monoxide poisoning is a chameleon in the medical world. Its symptoms mimic many other conditions, and there is not a single symptom that is the gold standard for all carbon monoxide poisoning. In other words, its symptoms are very difficult to identify, but there are several manifestations that you should be aware of.
Frequent symptoms
The most common symptoms of carbon monoxide poisoning are vague and associated with many conditions.
Early symptoms.
Carbon monoxide binds to hemoglobin, creating a molecule called carboxyhemoglobin (COHb), which interferes with the body's ability to transport and use oxygen, especially in the brain. Because of this, the symptoms are similar to other conditions that affect the brain and cause a decrease in oxygenation (known as "hypoxia"):
- headache;
- nausea;
- dizziness;
- fatigue.
Read also:Pneumocystis pneumonia (PCP) in HIV-infected people
Because it is a gas that tends to affect everyone who is exposed to it, carbon monoxide is easier to identify when symptoms affect more than one person. Due to its chameleon-like nature, it is still a daunting task, but headaches and nausea in individuality rarely makes anyone think of carbon monoxide poisoning as the most likely the culprit.
However, when carbon monoxide strikes multiple patients at once, it is often identified as “infection or poor diet,” rather than the assumption of carbon monoxide exposure.
Progressive symptoms.
As gas poisoning progresses, symptoms become more severe, but still extremely vague, and difficult to define as specific to carbon monoxide exposure:
- confusion of consciousness;
- shortness of breath;
- chest pain;
- vomit;
- blur or double vision;
- loss of consciousness.
There is no clear time frame to show how long it takes to go from headache to loss of consciousness. Exposure to carbon monoxide is time and concentration dependent, which means that the amount of carbon monoxide in the air is just as important as how long the patient is exposed to.
Rare symptoms
A deep red, flushed skin color (often referred to as cherry red) is one of the most telling signs of carbon monoxide poisoning. This is due to the high levels of carboxyhemoglobin in the blood.
Unfortunately, this bright red color is often found on postmortem examination. The level of carbon monoxide in the blood required to color the skin is so high that it is almost always fatal.
Thus, excessively reddened skin is too late a symptom to be useful in determining if a patient is suffering from carbon monoxide poisoning. For successful treatment, gas poisoning must be detected long before the patient's body turns bright red.
Complications and consequences

No matter how often gas poisoning occurs, much is still not clear about this condition. Long-term exposure to elevated levels of carbon monoxide - even if the levels are not so high, but exposure continues for days or weeks - may lead to peripheral disease arteries, cardiomyopathy and long-term, poorly understood neurological problems.
Brain damage is a serious problem that many people get from carbon monoxide poisoning. Patients may develop neurological complications (difficulty concentrating, loss memory, tremors, speech problems, etc.) simultaneously with carbon monoxide poisoning or later time. When neurologic signs and symptoms appear later, it is called delayed neurologic sequelae.
Research into why this happens and how to identify potential symptoms is still ongoing. For example, constriction of the pupil in the eye can predict how the brain will respond 30 days after exposure. One study that was conducted in patients for many years after they were exposed to monoxide carbon, showed that they are more likely to develop peripheral arterial disease than those who did not have a history of poisoning carbon monoxide.
Read also:Pneumothorax: Causes, Symptoms, Treatment and Prevention
There is very little evidence for a treatment for carbon monoxide poisoning. Most of the therapy options focus on removing carbon monoxide from the body as quickly as possible. These procedures range from basic high-precision oxygen delivery (15-25 liters per minute) to normal atmospheric pressure into the lungs and separation of carbon monoxide from hemoglobin to hyperbaric oxygen therapy at higher than usual atmospheric pressure.
When to see a doctor
Carbon monoxide poisoning is a very serious condition and always requires the help of a doctor. Carbon monoxide seeps into the bloodstream and takes up to several hours to remove.
Whenever carbon monoxide poisoning is suspected, call 112. Don't wait for help. Immediately move to fresh air. It is usually best to go outside while waiting for an ambulance.
When you see your doctor, note that history is more important than symptoms. The most important way to recognize carbon monoxide poisoning is to recognize the signs of the dangerous behavior that led to the symptoms.
Defective stoves, fireplaces, or wood-burning appliances are usually the culprit for carbon monoxide poisoning in the home. Cars and trucks are common culprits when working in a garage.
The doctor may ask you to describe how long it took for the symptoms to become severe enough to seek help. What was happening at this time? Was the weather cool, and someone from the family decided to start cooking kebabs in the yard? This information can help confirm that your symptoms are indeed carbon monoxide poisoning.
Diagnostics
If carbon monoxide is not recognized as the cause of symptoms, the problem may be misdiagnosed upon arrival at the emergency room. Therefore, it is important to inform the emergency doctor about your suspicions if you think CO is involved.
The diagnosis is relatively straightforward. It involves a non-invasive test with a device called a CO oximeter, which is placed on a finger, toe, or other part of the body. The oximeter contains two diodes that emit light beams of different wavelengths. The amount of light absorbed by the tissue can tell doctors how much carboxyhemoglobin (a compound created by the binding CO and hemoglobin) is in the blood.
Under normal circumstances, you would have less than 5 percent carboxyhemoglobin compared to free hemoglobin. Poisoning occurs if the level is between 10 and 30 percent. Death can occur at levels over 30 percent.
Conventional pulse oximeters are useless because they cannot distinguish between carboxyhemoglobin and oxyhemoglobin (a compound formed by the binding of oxygen and hemoglobin).
How is carbon monoxide poisoning treated?
Hemoglobin loves carbon monoxide and binds to carbon monoxide about 230 times more than oxygen, which is a problem because carbon monoxide does not provide any benefit to the body. Carbon monoxide poisoning in the air you breathe does not require a lot of carbon monoxide, and it takes a lot of oxygen to get rid of it, and that is where the treatment lies.
Read also:Pulmonary pleurisy: what is it, causes, symptoms and treatment
Traditional treatment
Carbon monoxide poisoning is not something you can treat at home. It takes at least 100 percent oxygen concentration for several hours to clear carbon monoxide from the bloodstream. Carbon monoxide poisoning - this is a situation that always requires a call to 112.
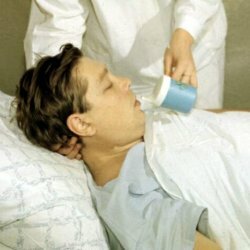
The main treatment for carbon monoxide poisoning is the introduction of high-precision oxygen using a breathing mask - oxygen masks with a plastic bag hanging from it - until carbon monoxide attached to hemoglobin is replaced by oxygen.
Half-life is a measure of the time it takes to eliminate half of a substance in the body. The half-life of carbon monoxide without the use of oxygen is 320 minutes - over five hours to halve the level. At this rate, the removal of carbon monoxide will take about a day.
Giving the patient 100 percent oxygen reduces the half-life to 74 minutes, which means that a patient with moderate exposure will still take more than five hours to reach acceptable levels of carbon monoxide in blood. Patients with carbon monoxide poisoning spend a lot of time sitting in the emergency room breathing pure oxygen.
Hyperbaric oxygen therapy

Another therapy option is to inject oxygen under pressure into a hyperbaric chamber, which essentially represents a round chamber in which the patient lies and inhales 100% oxygen at pressures 1.5-2 times higher than normal atmospheric pressure.
In a hyperbaric chamber, oxygen therapy can shorten the half-life of carbon monoxide to about 20 minutes.
Unfortunately, hyperbaric chambers are not always readily available, especially in rural areas. Even in areas where hyperbaric oxygen therapy is available, it can take a couple of hours to arrange treatment.
Given that the patient will receive conventional oxygen therapy during the waiting period, the benefit of faster treatment may already be lost. In addition, if multiple patients are exposed to carbon monoxide, then only one patient can be treated in the hyperbaric chamber at a time.
Prophylaxis
Proper use and maintenance of carbon monoxide emitting devices is the best way to avoid accidental carbon monoxide poisoning. In addition, recognizing the signs and symptoms of carbon monoxide poisoning, if possible, can be life-saving.
The most effective prevention at home is a carbon monoxide alarm. They are readily available online and at most hardware stores for between $ 20 and $ 80.