Lung infarction: symptoms, treatment and prognosis
 Lung infarction is the oxygen starvation of a portion of the lung tissue that is observed because oxygen carrying blood does not flow to the tissues.The obstruction to the blood flow in turn occurs due to the emergence of a barrier in a blood vessel that supplies a certain area of the pulmonary parenchyma.
Lung infarction is the oxygen starvation of a portion of the lung tissue that is observed because oxygen carrying blood does not flow to the tissues.The obstruction to the blood flow in turn occurs due to the emergence of a barrier in a blood vessel that supplies a certain area of the pulmonary parenchyma.
Essence of the disease
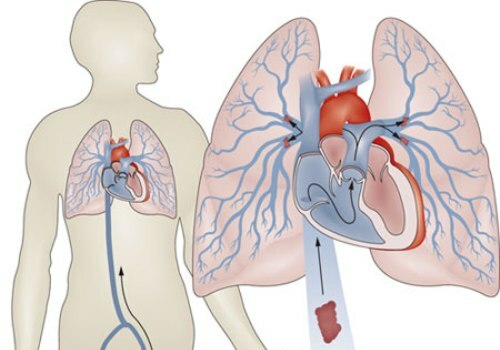
 Most often, oxygen starvation of the lung occurs due to thrombosis( formation of a blood clot on the inner wall of the artery occluding its lumen) or embolism( blockage by a foreign body brought with blood flow from anyA site of a human body - in this case it is called an embolus). Less common pathological process occurs because of squeezing the blood vessel from the outside.Lung infarction is also called pulmonary embolism, implying embolism of vessel obstruction in general, regardless of the blocking factor.
Most often, oxygen starvation of the lung occurs due to thrombosis( formation of a blood clot on the inner wall of the artery occluding its lumen) or embolism( blockage by a foreign body brought with blood flow from anyA site of a human body - in this case it is called an embolus). Less common pathological process occurs because of squeezing the blood vessel from the outside.Lung infarction is also called pulmonary embolism, implying embolism of vessel obstruction in general, regardless of the blocking factor.
By virtue of anatomical features, the lung infarction occurs on a restricted segment of the lung tissue , as the thrombus or embolus clogs individual arteries - lobar, segmental or smaller.Multiple embolisms can be subjected to vessels of small caliber, but they supply a small area of the lung - due to this the oxygen starvation of the organ is not total, but limited.
According to statistics:
- infarct of the right lung is observed 2 times more often than the left one;
- the lower lobes of the lungs are affected 4 times more often than the upper lobes.
Thus, is the most frequently infarcted location - the lower lobe of the right lung .Any pathology that develops in them( in particular, with severe symptomatology of tissue ischemia) should cause the alertness of pulmonologists every time, whether there is a lung infarction there.
Reasons
One of the main causes of the disease is pulmonary embolism( PE): due to it, there are 10 to 25% of clinical cases of a pulmonary infarction. It is suggested that they are in fact much larger - but often pathology is not detected during life due to erroneous diagnosis and is not confirmed after death due to medical ethics( the need to respond positively to the refusal of relatives of the deceased from his autopsy).At the moment, it is believed that due to pulmonary embolism of the pulmonary artery , a lethal outcome of a lung infarction occurs in 5-30% of patients with this disease .
PE is not only considered a pathology with a high probability of oxygen starvation of lung tissue - the risk of fatal cases due to lung infarction is even greater due to factors such as:
- no treatment;
- repeatedly recurrent thromboses - re-formation of a thrombus in the same vessel, often in the same place.The reason for the relapses is the physico-chemical compromise of the inner shell of the vessel;
- thromboembolism observed in the genus( burden of heredity by PE);
-
 age over 60;
age over 60; - reception of hormonal contraceptives;
- obesity;
- pancreatic tumors;
- pulmonary hypertension( increased pulmonary artery pressure);
- background( concomitant) diseases, worsening the general condition of the patient;
- misuse of intravenous catheters used for drip infusions( they can provoke thrombus formation at the injection site).
Sickle diseases, in particular:
- , sickle cell anemia( red blood cells have the shape of a sickle) are considered to be one of the most dangerous background diseases in terms of the appearance of PE and subsequent pulmonary infarction;
- DIC-syndrome( violation of the balance of the blood coagulation system, which leads to the formation of multiple thrombi).
In addition to PE, most clinical cases of lung infarction develop in patients who suffer from other cardiovascular diseases( in particular, chronic ones). First of all, these are cardiac pathologies, such as:
-
 atrial fibrillation( chaotic contraction of individual cardiac muscle fibers);
atrial fibrillation( chaotic contraction of individual cardiac muscle fibers); - mitral stenosis( narrowing of the left atrioventricular orifice of the heart);
- ischemic heart disease( cardiac muscle damage due to lack of oxygen);
- myocardial infarction as a complication of IHD( necrosis of the heart muscle);
- cardiomyopathies( lesions of various origin, except for blood supply disruption);
- infective endocarditis( infectious inflammation of the inner lining of the heart);
- atrial myxoma( benign tumor);
- heart failure;
- vasculitis( inflammation of vessels with their subsequent destruction)
and so on.
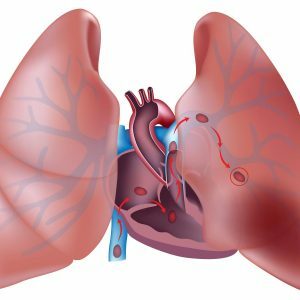
In the case of a heart pathology, thrombi in most cases are formed on the inner surface of the right atrial appendage.For some time they can be held in the place of formation, until the blood flow will not tear them away and carry in the artery a small circle of blood circulation, thanks to which the lungs are provided with blood.
For other reasons not related to cardiac disease, most often to pulmonary embolism that provokes a lung infarction, the following diseases and conditions can lead to:
- vein thrombosis( more often - deep) of the lower limbs;

- thrombophlebitis of deep pelvic veins;
- is a bed regimen prescribed in the postnatal or postoperative period, for serious illnesses or required due to the specifics of certain conditions( for example, the patient's stay in a coma);
- immobilization( immobilization) of the upper and lower extremities in fractures.
Bed rest and immobilization of limbs lasting even one week significantly increase the risk of thrombosis, which causes a lung infarction.
In the postoperative period, the risk of thrombosis with the development of a myocardial infarction is highest with:
- by cesarean section;
- operations on the organs of the abdominal cavity;
- gynecological interventions;
- operations on the thoracic cavity;
- hemorrhoidectomy( removal of hemorrhoids );
- surgery for varicose veins of the lower limbs, complicated by thrombosis or thrombophlebitis( inflammation of the vascular wall and the formation of a thrombus in this place).
Particularly dangerous thrombi that are attached to the inner surface of the vessel by a very small surface( in comparison with the entire surface area of its surface).Such thrombi are called floating( floating).They almost always come off and are carried by a current of blood into the lobar and segmental vessels of the lung.
In addition to the blood clot( thrombus), the embolus occluding the vessel can be:
- fatty particles;
- accumulation of tumor cells;
- clusters of microorganisms or fragments thereof;
- conglomerates of eggs of parasites caught in the flow of blood;
- gas bubbles.
Fat embolism of the blood vessels of the lungs can occur when:
- is mistakenly injected into the bloodstream of fatty suspensions( slurries);
- fracture of tubular bones - especially with polytrauma( multiple traumatic injuries - for example, in severe accidents), when several bones break, and the risk of embolization increases significantly.
Tumor embolus can theoretically cause cells of any tumors, but in the overwhelming majority of cases it is caused by cell clusters formed during the disintegration of malignant tumors at terminal stages.
If the place from where the embolus arrived is unknown, such a lung infarction is called primary, if it is determined - secondary.
Development of the disease
Classically, a lung infarction can develop from 2-3 hours to a day.After an acute period, salt joints are deposited in the affected tissue - the process is called the organization.It lasts no more than 7 days.
Due to the structure of the lung, its site, affected by lack of oxygen, resembles a pyramid( or wedge) in shape.Its apex is directed towards the root of the lung, and the base is in the opposite direction.
 As the affected tissue suffers from a lack of oxygen, it becomes dark cherry-colored, dense in consistency and bulges over adjacent healthy areas.Despite the fact that the blood supply to the pleura adjacent to the affected fragment of the lung does not suffer, it also changes - it becomes matte, and then dim, and bloody contents can accumulate in the corresponding part of the pleural cavity.
As the affected tissue suffers from a lack of oxygen, it becomes dark cherry-colored, dense in consistency and bulges over adjacent healthy areas.Despite the fact that the blood supply to the pleura adjacent to the affected fragment of the lung does not suffer, it also changes - it becomes matte, and then dim, and bloody contents can accumulate in the corresponding part of the pleural cavity.
Oxygen starvation of a fragment of the lung, which occurred due to obstruction of the branches of the pulmonary arteries, leads to the fact that the cells of the lung tissue begin to damage. It happens that from the neighboring areas of the lung with normal blood supply blood rushes here - the so-called hemorrhagic( blood) type of myocardial infarction develops.To the focus of the lesion infection often rushes, so when a lung infarction can join the so-called infarct-pneumonia, significantly complicating the course of the disease.
Lung infarction is not the final result of impaired blood flow.Its possible outcomes are:
- resorption( resorption of the altered oxygen starvation tissue);
- infiltration changes( compaction);
- scarring;
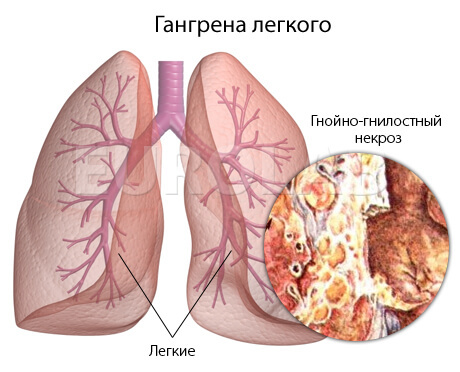
- abscess( suppuration) of the affected area of the lung;
- gangrene( destruction) of lung tissue.
Symptoms of a pulmonary infarction
Symptoms of a heart attack depend on the level of occlusion of the blood vessel.It can be of the following types:
- embolism of small branches of the pulmonary arteries;
- submissive( emboli hammers branches that are responsible for blood supply to segments of the lung or whole parts thereof);
- massive( blockage of the central trunk of the pulmonary artery or its main branches).
These criteria distinguish such types of infarction of the lung as:
- limited - clogged those branches of the pulmonary artery that provide blood to the segments of the lung and its smaller areas;
- is extensive - larger vessels or many smaller( multiple embolism) are affected.
Symptoms of myocardial infarction do not develop immediately after clogging of the blood vessel, they begin to appear clearly on average 2-3 days after the blockage. The main clinical signs of the disease:
- chest pain;
-
 hemoptysis - separation of sputum with a trace of blood( "rusty sputum");
hemoptysis - separation of sputum with a trace of blood( "rusty sputum"); - increased body temperature;
- with pronounced hyperthermia, shortness of breath( up to 20 breaths per minute) and heart rate increase( more than 100 beats per minute);
- pallor, and then cyanosis( cyanosis) of the skin and visible mucous membranes;
- there may be interruptions in the operation of the heart of an arrhythmic nature, as well as a decrease in blood pressure - in critical cases with the development of a collapse( sudden development of cardiovascular insufficiency).
Chest pain with a pulmonary infarction has the following characteristics :
- acute;
- intensive( similar in part to the pain with angina pectoris);
- intensifies with activities - coughing, trying to breathe deeper, tilting the trunk.
Pain sensations mean that the pleura is affected( the lung tissue itself does not hurt) - the so-called reactive pleurisy develops at the site of the affected lung fragment, and about half of patients with a lung infarction suffer from it.
Hemoptysis is seen in almost half of patients with a lung infarction .In 5-6% of patients, pulmonary hemorrhage is possible.
Hyperthermia ranges from 37.1 to 37.8 degrees Celsius.It is able to withstand a long time - up to 2 weeks.If the infarct-pneumonia has developed - the body temperature can rise to 39 degrees Celsius.
It should be remembered that with a lung infarction, symptoms can develop not only in the cardiovascular and respiratory, but also in other organs and systems - first of all:
- of the brain;
- digestive system.
Possible cerebral disorders:
- syncope;
- convulsions;
- coma.
Symptoms of the side of the gastrointestinal tract:
- nausea;
- vomiting, not associated with food intake;
- jaundice( it occurs because of secondary changes in the hepatic tissue that lead to the breakdown of hemoglobin).
If an affected area of the lung, located close to the diaphragmatic pleura, signs of an acute abdomen may appear - primarily severe abdominal pain and bowel movement.
Lung infarction can be:
- uncomplicated;
- complicated.
The most common complications of this pathology are:
- bacterial pneumonia;
- candidiasis( fungal infection);
- lung abscess( limited suppuration);
- gangrene( necrosis) of the lung;
- pleural empyema( suppuration with fuzzy boundaries);
- sepsis( total infectious disease of the body).
Diagnosis of myocardial infarction
A pulmonary infarction is diagnosed by a joint effort of a pulmonologist and cardiologist. The diagnosis is based on complaints, given physical examination( examination, feeling of the chest, its tapping and listening to the phonendoscope) and the results of additional research methods.
With a lung infarction, a number of instrumental methods of investigation are informative:
-
 radiograph of the lungs in two projections - in the picture one can see the same "wedge" of lung tissue, affected by lack of oxygen, as well as fluid in the pleural cavity;
radiograph of the lungs in two projections - in the picture one can see the same "wedge" of lung tissue, affected by lack of oxygen, as well as fluid in the pleural cavity; - computed tomography and its more progressive version of multispiral computed tomography( MSCT) - the results will be the same as for radiography;
- ECG - signs of an overload of the right side of the heart;
- echocardiography( echocardiography) - during it, signs are revealed( also called echocardiograms) of increasing blood pressure in the pulmonary artery, as well as thrombi in the enlarged right heart;
- ultrasound dopplerography of the veins of the lower extremities( UZDG), or ultrasound of the vessels - with its help can detect thrombi in the veins of the lower extremities;
- angiopulmonography - it demonstrates blockage of the branches of the pulmonary artery;
- lung scintigraphy - with the help of this method confirm the deterioration of the blood supply to the lung tissue.
Laboratory test methods used in the diagnosis of pulmonary infarction are:
- general blood test - a moderate increase in the number of white blood cells is diagnosed as a reaction to "spoiled" lung cells;
- biochemical blood test - it will increase lactate dehydrogenase( formed during cellular respiration) and total bilirubin( due to the breakdown of hemoglobin in the secondary affected liver);
- analysis of the gas composition of blood - a decrease in the amount of oxygen is recorded.
Differential diagnosis
Because of the similarity of the signs of a pulmonary infarction, it should be distinguished from such diseases as:
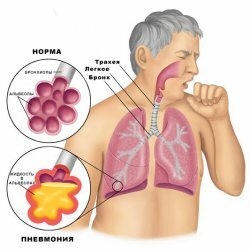
- croupous pneumonia( inflammation of the lungs with the formation of fluid in the alveoli);
- spontaneous pneumothorax( the appearance of no apparent causes of air in the pleural cavity);
- atelectasis( falling off) of the lung;
- myocardial infarction( necrosis of the heart muscle due to lack of oxygen);
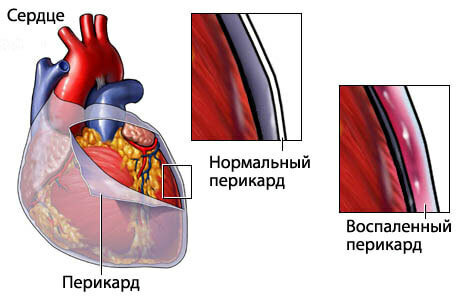
- pericarditis( inflammation of the heart shave);
- myocarditis( inflammation of the heart muscle of various origin);
- fracture of
ribs and some others.
Treatment of a pulmonary infarction
Treatment for a lung infarction consists of:
- first aid;
- treatment in a hospital.
Due to the fact that oxygen starvation of the lungs is fraught with the whole organism, treatment of a lung infarction should be started in an emergency.
As a first aid, a pain syndrome is stopped - for this purpose, strong non-narcotic or narcotic painkillers are injected.The patient is immediately taken to the intensive care unit.
The first medical task for lung infarction:
- to eliminate the existing thrombus;
- prevent subsequent thrombosis;
- increase blood pressure, which is reduced due to blockage of the pulmonary artery.
Fibrinolytic agents are used to destroy( dissolve) the already formed thrombi.
To prevent recurrent thrombus formation, anticoagulants are used:
- direct action( including heparin);
- indirect action.
Anticoagulants should be administered under the constant control of the coagulogram in order not to provoke bleeding . It must be remembered that they have contraindications for use - this is:
- internal bleeding of any origin;
- peptic ulcer of stomach and duodenum;
- hemorrhagic diathesis( increased tissue bleeding);
- malignant tumors of different localization.
 For arterial hypotension, drugs that narrow the vessels are administered, and intravenous drip infusion solutions are administered.
For arterial hypotension, drugs that narrow the vessels are administered, and intravenous drip infusion solutions are administered.
For the treatment, as well as the prevention of infarction pneumonia, antibiotics of a wide spectrum of action are prescribed.
An extremely important treatment for lung infarction is inhalation of oxygen.
If all these methods did not produce the desired effect, the question is raised about the operative extraction of a thrombus from the pulmonary artery - thrombectomy . During this operation, a special filter is also inserted into the system of the inferior vena cava, which will later "screen out" thrombi.
When blocking the branches of the pulmonary artery by other emboli treatment is almost the same.Including injections of drugs that prevent the formation of blood clots - with embolism of any origin can develop coagulopathy( a violation of blood clotting).
Prevention
To prevent lung infarction, all factors that can cause pulmonary congestion should be avoided. Since in most cases, embolization causes a thrombus, a lifestyle that excludes thrombosis or at least reduces its risk should be followed:
- timely provide medical care for signs of thrombophlebitis( especially with varicose veins of the lower extremities);
- when using lower limb veins, use knitted underwear( special elastic stockings) or, at least, make bandages with elastic bandages( archaic method, but less expensive);
- after surgical interventions do not ignore the practice of conventional medical gymnastics, hoping only for medicines;
- , as far as possible after operations, practice early recovery;
- observe the timing of the use of intravenous catheters for drip administration of drugs;
- quit smoking( causing vasoconstriction, nicotine exacerbating the course of a lung infarction).
Prognosis for lung infarction
The prognosis for lung infarction is rather complicated: delay in diagnosis and treatment can lead to irreversible destruction of lung tissue . Threats to the health and life of the patient can be avoided due to timely diagnosis and emergency medical measures.
The risk for health and life associated with lung infarction is increased under the following conditions:
- Severe chronic cardiovascular failure;
- complications( infarct-pneumonia, abscess and gangrene of the lung, sepsis);
- recurring cases of pulmonary embolism.
Kovtonyuk Oksana Vladimirovna, medical reviewer, surgeon, consulting physician