Bleeding during pregnancy at late stages: possible causes and diagnosis

Bleeding at late pregnancy - a series of bleeding that opens after 28 weeks of pregnancy.In most cases, they are a sign of a formidable complication and require emergency medical care.The causes of blood discharge in the second half of pregnancy are most often associated with placental pathologies.In this case, there are also situations where bleeding is absolutely not related to the pregnancy itself, but only the doctor can differentiate the diagnosis correctly.
Note: very rarely bleeds open in the 2nd trimester because of complications associated with pregnancy.Its cause is usually the fall of a woman or a strong blow to the abdomen, unlike the 3rd trimester, when this happens against a backdrop of formidable pathologies.
Causes of bleeding in late pregnancy
In later terms, bleeding can trigger such causes :
- placenta previa;
- detachment of the normally located placenta( premature);
- uterine rupture;
- bleeding from the fetal vessels.
Late bleeding due to placenta previa: symptoms, causes, treatment

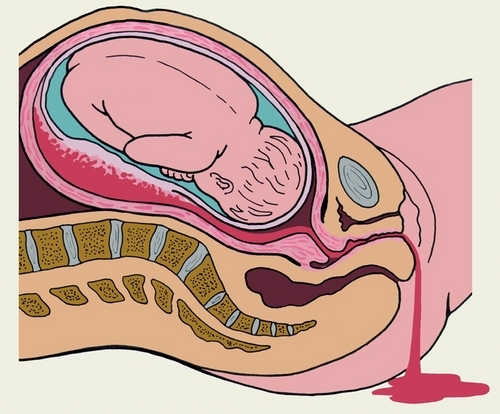
This condition is characterized by an atypical location of the placenta in the uterine cavity.Placenta prediction means that when an ultrasound is diagnosed, the doctor notices its abnormal location in the lower segment of the uterus, while it should be on its side wall or in the bottom.The placenta in this case partially or completely overlaps the internal pharynx.There are 2 variants of presentation: incomplete and complete, as well as low location of the placenta( below 5 cm from the throat).
Important: this pathology is the cause of for high perinatal mortality of children, because of it premature birth often occurs.As a result, babies are born premature, with a syndrome of respiratory distress, etc.Also, it increases the risk of hemorrhagic shock and death in the mother.
This severe complication can result from pathological changes in the endometrium or normal implantation of the fetal egg.
In particular, such provocative factors of placenta previa and associated hemorrhage are identified in the late term :
- anomalies in the structure of the uterus;
- second, third, etc.Childbirth;
- abortion;
- uterine underdevelopment;
- is a multiple pregnancy;
- uterine perforation;
- uterine myoma;
- diagnostic scraping;
- endometriosis;Caesarean section. .
Clinically, the placenta previa is manifested by the bleeding of a different abundance without pain, which can suddenly stop and also suddenly resume.The second symptom - hypoxia of the fetus - because of violations in hemodynamics, a child in the womb of the mother does not receive the necessary amount of nutrients and he develops oxygen starvation.
Depending on where the placenta is located in the uterus, bleeding can begin both during child bearing( full presentation) and during delivery( incomplete, low attachment).A low-lying placenta is indicated by a postnatal examination of the afterbirth, on which a small distance between the rupture of the membranes and the placenta itself is noticed.
Important: treatment of this condition and accompanying bleeding in late pregnancy should be carried out exclusively in a hospital setting, and it can be prompt or medically.
Conservative therapy is suitable for unhealthy bleeding, normal blood pressure and satisfactory blood test.
In addition to strictest bed rest, the patient is also prescribed :
- preparations for preventing fetal hypoxia;
- blood transfusion( erythrocyte mass, fresh-frozen plasma);
- medicines for removing the increased tone of the uterus;
- means for the normalization of utero-placental blood flow;
- Vitamins C, E, K.
The delivery in a patient with bleeding with placenta presentation( complete and incomplete) is always performed in an operative way in the form of a caesarean section.A direct indication for him is the massive blood loss, the immaturity of the mother's birthmarks.
Sometimes a pregnant woman with incompleteness of the placenta is allowed into labor.If she has a normal labor activity, there is a dilating cervix for 3 fingers, then the doctor opens the fetal bladder.Thanks to this, the fetal head descends into the small pelvis and mechanically presses the area of placental abruption, which stops the bleeding.
Complete algorithm for the treatment of bleeding with placenta previa look at the diagram:
Causes, symptoms and treatment of bleeding during uterine rupture
 Bleeding in late pregnancy can develop as a result of rupture of the uterus. This complication is formed due to such reasons :
Bleeding in late pregnancy can develop as a result of rupture of the uterus. This complication is formed due to such reasons :
- cesarean section in history( scar on uterus);
- bladder skid;
- chorioepithelioma.
Very often, the rupture of the uterus is due to a fresh scar on it, which did not have time to fully heal after the first pregnancy.
Note: , the optimal interval between pregnancies should be 2.5 to 4 years, especially if the first child was born by cesarean section.The scar on the uterus should fully heal until the next pregnancy, which takes at least 2-3 years.
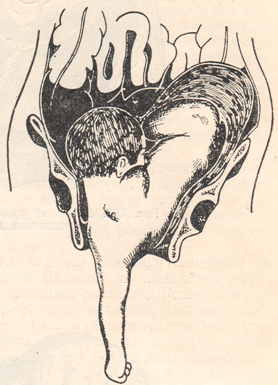
When the uterus ruptures, internal and external bleeding occurs.A woman complains of acute pain in the abdomen, spotting during pregnancy( bright scarlet).This symptomatology indicates that the hemorrhagic shock pattern is developing.The mechanism of rupture of the uterus is quite simple: it is excessively stretched, its walls are thinned, and the area of the attachment site of the placental area increases, resulting in a rupture of the muscular layer.
The condition is very dangerous, therefore it requires immediate first aid measures.
To stop bleeding and treat pathology, use:
- laparotomy,
- rupture or complete amputation of the uterus,
- replenishment of lost blood volume.
Bleeding in premature detachment of a normally located placenta
This is a condition in which a normally located placenta exfoliates before the fetus is born during pregnancy or in childbirth until the 3 rd period, when this should occur normally.This pathological process is always accompanied by external, internal or combined bleeding.It can cause death and fetus, and the mother as a result of hemorrhagic shock due to blood loss and the multiple organ dysfunction that developed due to it.
The causes of such bleeding in late pregnancy can be:
- rapid outpouring of amniotic fluid;
- hypovitaminosis of different types;
- syphilis;
- abnormality in the placental circulation;
- eclampsia;
- hypotonic and hypertensive disease;
- short umbilical cord;
- large fruit;
- external obstetric turn;
- heart disease;
- severe gestosis;
- endomyometritis;
- polyhydramnios;
- amniocentesis;
- abnormalities of the development of the uterus;
- trauma( fall);
- thyrotoxicosis;
- late rupture of membranes;
- tuberculosis;
- pregnancy recurrence;
- stress.
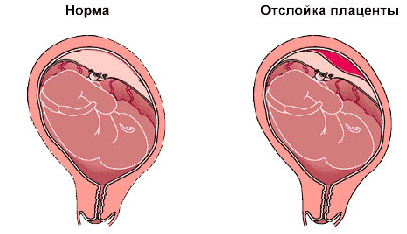
The placental abruption is of two kinds: :
- is complete when the whole placenta exfoliates completely;
- partial, in which only part of the posterior is separated from the wall of the uterus at its center or edge, and may have a non-progressive and progressive course.
Changes in the endothelium and an increase in the permeability of the vascular wall are observed at the placental level.

The most dangerous situation develops with a progressive detachment, which does not give external bleeding.The blood that accumulates between the placenta and the uterus wall forms the hematoma, and it rapidly increases.The uterus stretches, and the blood begins to penetrate into her muscular layer and the placenta.As a result, the walls of the uterus are impregnated with blood, which causes cracks on them.Blood enters the peritoneal tissue and into the abdominal cavity.The uterus itself acquires a cyanotic color with hemorrhages on its surface.This complication of bleeding is indicated with premature detachment of the normally located placenta - "Queen of the Queen", after the author's name for the first time described it.
Symptoms accompanying bleeding during late pregnancy in this pathology:
- pain syndrome with abdominal localization;
- bleeding;
- increased uterine tone;
- fetal hypoxia in the acute stage.
The medical tactics and necessary treatment depend on the area of detachment, the level of blood loss, the condition of the woman and the fetus, the gestation period.If this complication occurs during pregnancy, then resort to a caesarean section in an emergency, no matter what trimester and in what state the fetus is.
In case when the "Queen of the Queen" is diagnosed during the operation, 2 options for further action are possible: the first is an extirpation of the uterus with massive bleeding.Preservation of the uterus became real after the emergence of high technologies in modern medicine.If there is a vascular surgeon and special equipment for intraoperativeinfusion of anatomical blood in the brigade, it is possible to keep the uterus in the patient, but at the same time bind internal iliac arteries.
In the case of a stable condition of a woman and fetus with a gestation period of up to 34 weeks, absence of massive bleeding( a small retroplacental hematoma without progression is allowed according to the USP data), severe expectant anemia can be used.
The woman and the fetus must be under constant medical supervision, which includes activities such as :
- doppler;
- cardiotocography;
- strict bed rest;
- reception of antispasmodics;
- reception of disaggregants;
- reception of multivitamins;
- anemia therapy;
- transfusion of freshly frozen plasma( according to indications).
Bleeding from fetal vessels
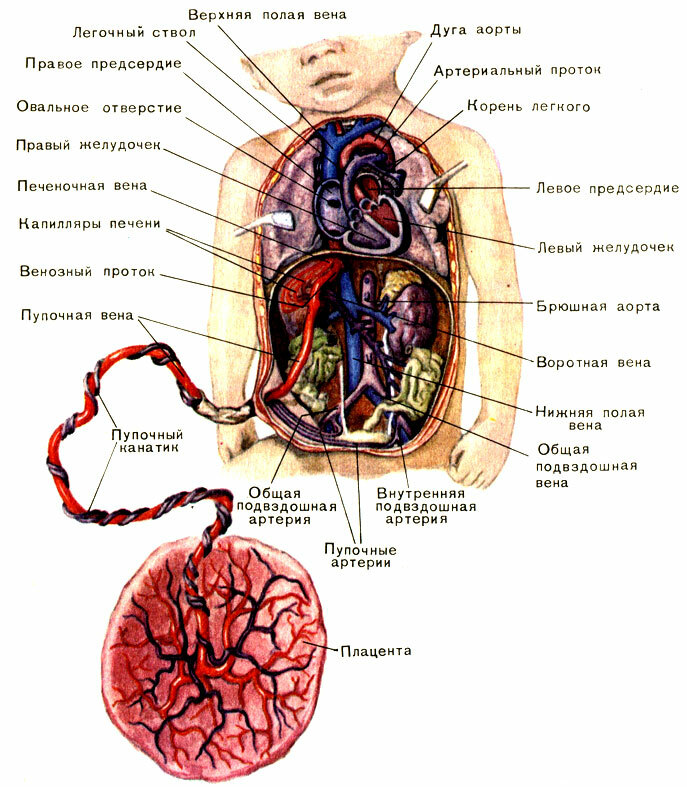
This pathology occurs in 1 case for 5000 pregnancies.Bleeding from the umbilical cord can develop with their atypical shell attachment.To put this diagnosis is difficult.
Tumor cord or umbilical cord injury manifests itself by such symptoms:
- increased fetal heart rate, which is gradually replaced by its decrease;
- acute fetal hypoxia;
- the woman has a bleeding of bright scarlet color without pain syndrome and an increased tone of the uterus.
This pathology has a very high risk of antenatal fetal death.Only a doctor in the competence to decide whether to maintain a pregnancy and how to perform the delivery.
Bloody discharge during pregnancy not related to pregnancy itself: causes and treatment
It is worth mentioning that there are a number of reasons that can also cause bleeding in a future mother, but they are not related to the pregnancy itself.Such secretions provoke a variety of factors, and to determine them, it is important to consult a doctor for help immediately after the appearance of the first signs of bleeding.
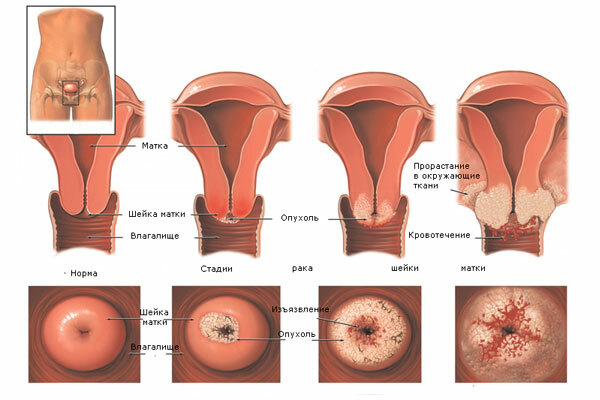
Bleeding in advanced stages of pregnancy can cause :
- Cervical erosion;
- cervical ectopia;
- cervical polyp;
- cervical cancer.
Bleeding during ectopy and cervical erosion during pregnancy
Such a combination is not pleasant, but it often takes place for a pregnant woman discreetly.There will be bloody discharge, which the doctor connects directly with erosion, can during the first period of childbirth.With the disclosure of the erosive cervix, the risk of its rupture in childbirth rises at times.But during pregnancy this pathology is not cauterized as usual, as this complicates the course of future births, but is treated conservatively.This tactic will avoid infection of the wound surface on the cervix.
Bloody discharge in cervical polyps
Very rarely, they provoke bleeding during pregnancy, but this fact is known.Treatment consists of removal of the polyp and the appointment of haemostatic drugs.
Bloody discharge in cervical cancer
This combination in pregnant women is not common, since the disease itself develops after 40 years of age, with a history of abortion, childbirth and promiscuity.When opening bleeding due to cancer, the cervix is resorted exclusively to surgical treatment.During the intervention, the woman gives birth and completely removes the uterus.
Viktorova Julia, obstetrician-gynecologist



