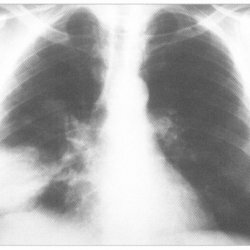
Candidiasis pneumonia, or invasive candidiasis of the lungs
 Invasive pulmonary candidiasis is common under the concise definition of candidiasis pneumonia. This disease is most often manifested by acute disseminated candidiasis. Isolated candidiasis pneumonia is rare, it is possible with prolonged agranulocytosis or with aspiration of gastric contents. Candidiasis( also moniliasis, condylidiasis, candidymycosis, candidiasis) is anthroponous mycosis, which is accompanied by signs of tissue damage by yeast-like micromycetes of the Candida species. Candida is determined by sputum collection. Most often, its presence is detected in patients with acute chronic nonspecific lung diseases( in 50% of cases) and in patients with pulmonary tuberculosis( in 60% of cases).
Invasive pulmonary candidiasis is common under the concise definition of candidiasis pneumonia. This disease is most often manifested by acute disseminated candidiasis. Isolated candidiasis pneumonia is rare, it is possible with prolonged agranulocytosis or with aspiration of gastric contents. Candidiasis( also moniliasis, condylidiasis, candidymycosis, candidiasis) is anthroponous mycosis, which is accompanied by signs of tissue damage by yeast-like micromycetes of the Candida species. Candida is determined by sputum collection. Most often, its presence is detected in patients with acute chronic nonspecific lung diseases( in 50% of cases) and in patients with pulmonary tuberculosis( in 60% of cases).
Candida fungi are part of the normal microflora of the oral cavity, colon, gastrointestinal tract, vagina, often and the nasopharynx, rarely the skin.
A fairly serious problem if candidiasis pneumonia develops in immunocompromised patients( complications in 90% of cases).In the presence of candidal mucosal lesions in oncohematological patients with neutropenia in the case of not carrying out appropriate treatment, the disease acquires a progressive character. In febrile patients with neutropenia not responding to broad-spectrum antibiotic therapy, there is a high risk of clinically significant pulmonary candidiasis( in 20% of cases).
Frequent outbreaks of candidiasis occur among working baths, vegetable canneries, confectionery factories, as well as in children's institutions. Many people have an allergy to Candida fungi, it is expressed in a certain reaction of patients with the use of wine, beer, yeast bread, champagne.
Pathogenesis of Candidiasis
There are five consecutive phases in the pathogenesis of candidiasis:
- adhesion of micromycetes on the surface of epithelial barriers;
- pathogen significantly increases in quantity and penetrates through the epithelium;
- , Candida interacts with cellular elements of connective tissue;
- Candida fungi penetrate the vascular bed;
- dissemination of the pathogen on the body with sequential formation in the respiratory system of candidiasis lesions.
Cases with the development of all phases of mycosis are found in patients with deep disorders of the immune system. The development of acute candidiasis pneumonia is possible as a result of a downward infection that changes from bronchial or as a result of lymphohematogenous seeding.
Clinical picture of
There are two types of invasive pulmonary candidiasis:
- primary candidiasis pneumonia. Formed in the lungs with aspiration of the pathogen, it develops quite rarely;
- secondary candidiasis pneumonia. It arises as a result of hematogenous dissemination of Candida spp from other sources. It occurs in 14-40% of patients with acute disseminated candidiasis.
It is very important to distinguish invasive pulmonary candidiasis with a characteristic high percentage of death, from a safer surface candidiasis of bronchi and trachea. It is also possible to become confused when determining the final diagnosis of candidiasis of the lungs in comparison with the most often not requiring treatment of superficial colonization of the respiratory tract. Along with all of the above, airway colonization and superficial candidiasis are often accompanied by the presence of invasive candidiasis in patients.
The most common symptoms of pulmonary candidiasis are:
- hemoptysis;
- febrile body temperature;
- shortness of breath;
- cough;
- characteristic pain in the thoracic region.
There are also quite often cases when invasive candidiasis of the lungs develops without the presence of the above symptoms. This situation can occur if the patient is in serious condition or is being carried out by mechanical ventilation. Clinical presentation of the disease can vary greatly depending on the risk factor, the patient's immune status, the main disease, the anatomical localization of the infection and its spread.
There are two forms of Candida pneumonia, namely: acute form;Chronic form - observed in adults, is most often not seen against the background of any inflammatory disease of the respiratory tract, antibiotic treatment worsens the general condition of the patient, increased dyspnoea, cough.
For the acute form of candidiasis with lung lesions, the following characteristics are characteristic:
- , the culture of Candida fungi is isolated in blood tests and other, biologically sterile liquids;
- positive serological test results;
- observed the presence of foci-screenings on the skin of the patient;
- determination of the filamentous form of the pathogen in pathological materials;
- , when examining the fundus, there are foci of white or yellowish hue;
- in the computed tomography of the lungs there is a large number of small, miliary foci located along the periphery;
- the presence of dry cough, when examining rales is not observed;
- when carrying out computer studies by ultrasound, there is a presence of foci of destruction up to 2 cm in the spleen, liver, etc.;
- the presence of Candida mushrooms in two sputum cultures made at different times;
- resistant fever or its return to the background of antibiotic treatment of a wide spectrum.
Treatment of
There are definite indications for the onset of antifungal therapy in patients without neutroperia:
- development of candida of several loci;
- presence of a large number of risk factors.
The goal of the treatment is to eliminate clinical and laboratory signs and symptoms of the disease, while reducing the risk of relapse.
For invasive candidiasis of the lungs without neutropenia, the following types of treatment are used:
- fluconazole, administered at 400 mg / day;
- amphotericin B, 0.5-1.0 mg / kg / day;
- caspofungin, the first dose is 70 mg, then 50 mg / day;
- liposomal amphotericin B, 5 mg / kg / day;
- lipid complex of amphotericin B, 5 mg / kg / day.
If the sensitivity of C. Glabrata is low to fluconazole, an increase in the dose to 800 mg / day is permitted, or the drug can be changed and amphotericin B or caspofungin used. Caspofungin is a strong enough drug for many species of Candida.
For invasive candidiasis of the lungs with neutropenia, amphotericin B, or a variety of its forms at the same dosages, is most often prescribed. Fluconazole and amphotericin B have a good property of penetration into the pleural cavity. Proceeding from this, carrying out intrapleural injections of these drugs is not advisable.
In the presence of disseminated candidiasis, febrile patients without neutropenia undergo empirical therapy. It includes the use of amphitericin B intravenously, as well as fluconazole, orally or intravenously.
In immunocompetent people in the presence of catheter-dependent fungemia, catheter removal is performed and intravenous medications are prescribed:
- caspofungin, the first dose is 70 mg, further 50 mg / day;
- amphotericin B, 0.5-1.0 mg / kg / day;
- fluconazole, 400 mg / day.



