Neurotoxicosis in children, clinic, diagnosis, treatment

Neurotoxicosis in children: etiology and pathogenesis.
Neurotoxicosis has the nature of polyethic. A common cause for neurotoxicosis is viral infection( acute respiratory viral infection, influenza, adenovirus infection) and bacterial diseases( escherichiosis, shigillosis, food poisoning, salmonellosis, etc.).With neurotoxicosis, any neuroinfection( encephalitis of various etiologies, meningitis) can begin.
The main mechanism pathogenetic in the development of this disease is the damage of the generalized terminal vascular bed in the autonomic and central nervous system. Effects on the wall of blood vessels, toxins and an infectious agent, lead to disturbances of vascular circulatory, hypoxia and increased vascular permeability. This change is diffuse. More important is the violation of the external vegetative center of the hypothalamus, which has increased sensitivity to various effects. Violation of the nervous regulation leads to the emergence of a number of neurological disorders, poor peripheral blood flow, a violation of thermoregulation, metabolic shifts and other disorders.
Neurotoxicosis: a clinic.
The clinical picture is polymorphic: at first it is violent, acute, the patient is agitated, then comes the oppression of consciousness, which can grow into a coma. At times, the onset of the disease is accompanied by vomiting, often that is repeated, and this is not related to the nature and intake of food. During the mid-cerebral coma, the tone in the sympathetic nervous system may sharply increase, within a few hours the body temperature rises or reaches high figures at once( 39-40C).During this period, stiff neck muscles, tension in a large fontanel, and in older children, symptoms of Brudzinsky and Kernig can be noted. Breathing is rapid, superficial and intermittent. In a number of cases cardiovascular disorders may predominate;Hypertension arterial with a small pulse amplitude, manifested tachycardia, increased permeability at the walls of blood vessels, which can develop pulmonary and brain edema, convulsive syndrome. With ineffective measures or with no medical measures taken at all, the shock state begins to develop: the blood pressure drops, the skin begins to acquire a grayish shade, the tone of the heart becomes deaf, the tachycardia replaces the bradycardia, oliguria up to the anuria( "trunk" coma), the paresis as an intestine, And sphincters with involuntary urination and defecation. With more light neurotoxicosis, hyperventilation syndrome or hyperthermia predominate.
Neurotoxicosis in children: diagnosis.
Diagnosis of one of the leading clinical syndromes of neurotoxicosis, with symptomatic of a certain nature, is not difficult, but it is very necessary, no matter what the etiology of the disease, since diagnosis allows choosing tactics for emergency care and provides an opportunity to prevent the development of neurotoxicosis in severe form with varying degrees of consciousness disorder fromSomneventnosti and up to a coma.
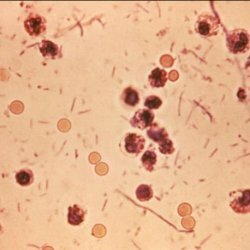
Differential diagnosis is performed with such neuroinfections as meningitis and encephalitis. Clinically, the encephalic reaction and meningism with neurotoxicosis are difficult to distinguish without research of cerebrospinal fluid. With lumbar puncture, all patients with neurotoxicosis noticed increased intracranial pressure up to 250 mm due to the fact that there is an irritation of the vascular plexuses with the hyperproduction of the cerebrospinal fluid and impaired its absorption.
There is no pleocytosis completely in the cerebrospinal fluid, the protein concentration is often below 0.17.
The peculiarity of the encephalic and meningeal response of neurotoxicosis should be considered, rapid( within 1-2 days) decrease in intoxication and a drop in temperature, in the underlying disease, and disappearance of these reactions.
Neurotoxicosis: treatment.
A sick child should be urgently hospitalized in the intensive care unit and intensive care unit. An emergency caregiver needs, in the stage of indemnification of toxicosis, to give the patient an elevated position, cramping, dehydration( intramuscularly 25% of magnesium sulfate 0.2 ml / kg), administration of vascular agents( intramuscular 2% papaverine solution 0.15-1 ml / kgTogether with 1% dibazol solution of 0.1-0.5 ml, for both drugs the average dose is 1-2 mg for each year of life).It is also necessary to introduce a broad spectrum of action of antibiotics and calcium preparations, analgesics for hyperthermia, seduksen with seizures.