Herpes zoster: clinic, diagnosis, treatment
 Herpes zoster is an acute viral disease, manifests itself as erythematous-vesicular group rashes, arranged along the direction of the nerve trunks and accompanied by severe neuralgic pains. The causative agent of this disease is the virus varicella-zoster - a dermatoneurotropic virus. The more dangerous the herpes zoster, the clinic, the diagnosis, the treatment of which is described below, we will discuss in this article.
Herpes zoster is an acute viral disease, manifests itself as erythematous-vesicular group rashes, arranged along the direction of the nerve trunks and accompanied by severe neuralgic pains. The causative agent of this disease is the virus varicella-zoster - a dermatoneurotropic virus. The more dangerous the herpes zoster, the clinic, the diagnosis, the treatment of which is described below, we will discuss in this article.
Routes of infection - airborne and contact. Adults, in contact with a patient, rarely "pick up" the disease. What can not be said about children, in contact with patients, they can begin to develop chicken pox. Characterized herpes zoster sporadic. Epidemics are not observed, although with the onset of autumn and spring, the number of patients begins to increase.
The mechanism of development and pathological processes of herpes zoster until the end is not clear, however, modern views allow us to treat herpes zoster as a secondary infection, which is caused by a partial decrease in immunity, developed due to the virus that the organism contacted in the past.
It is believed that the latent state of the virus is located in the nerve ganglia, but as soon as the reactivation occurs, the infection begins to move in the direction of the nerve to the skin, causing rashes.
In practically healthy people, the disease develops without any visible predisposing factors. Meanwhile, the infection can be triggered by trauma, x-ray exposure, hypothermia, immune deficiency and a number of other factors. Especially it would be desirable to note the development of this disease in people with leukemia and malignant tumors.
Herpes simplex herpes zoster differs in that it does not recur. Recently, relapses of this disease have been observed in patients with HIV infection, and then in the late stages.
Herpes zoster: clinic
The disease in such cases begins with painful sensations in the place of the forthcoming localization of the rash. The pains are different in intensity, and given the fact that at the initial stage( the first days of onset of the disease), there are no changes from the skin, they are regarded as a manifestation of another disease, for example, angina pectoris, pneumonia, renal colic.
After about 4 days on the site of the appearance of pain, there is hyperemia and swelling of the skin, because of what small knotty elements begin to form by the group. They do not stay long in this state, because they turn into bubbles, in which you can see the transparent content. As a rule, the bubbles appear "jerky", so at the height of the disease you can observe the rashes at different stages of development.
The process is located on a large area, it has a one-sided character. Usually localized in the direction of the nerves, often in the chest, less often located on the site of innervation of the trigeminal nerve, lumbosacral region, on the skin of the neck, limbs, along the ear, facial, auditory nerves. Almost 100% of patients have regional lymphadenopathy.
Most of the bubbles, drying up, turns into crusts, and some either spontaneously, or as a result of a trauma to the surface of the bubble is opened, forming erosion. After the crust has disappeared, and the epithelization of erosions has occurred, the process ends, leaving a temporary redness after itself. On average, the duration of the disease is two to three weeks.
Painful sensations in herpes zoster
Often, rashes are accompanied by general weakness, malaise, nausea, headaches, fever. It is not uncommon for cases when deviations are observed that are identical to the typical course of the disease. This, above all, refers to the main subjective symptom - pain. Painful sensations can occur simultaneously with a rash, or after a rash, sometimes there is no pain at all.
Pain in its intensity are different: barely perceptible paresthesias can develop into debilitating, painfully cutting pains, which can be removed only by the introduction of drugs and then for a short period.
Postherpetic neuralgia is not excluded, which, after the disappearance of the rashes, for a long time( from several months to several years) are accompanied by severe pain.
Rashes are not typical. Vesicles become large, reaching in some cases the size of the plum( usually the bubbles do not exceed the size of a pea), in which case the herpes zoster is bullous. Also in the bubbles is not a clear liquid, and bloody liquid, when dried, hemorrhagic crusts are formed, in which case herpes zoster is hemorrhagic.
The most severe course and persistent skin changes is the herpes zoster, which wears a gangrenous form. This form of herpes in the process involves deep layers of the skin. Sometimes the disease occurs without the appearance of vesicles, that is, abortively.
Shingles: Diagnosis
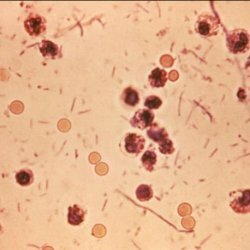
It is not difficult to diagnose the typical form of herpes zoster. If necessary, laboratory diagnostics is used, which allows isolating the virus on cell cultures, as well as cytology.
Herpes zoster from herpes simplex is characterized by sharp pain, no recurrence and unilateral spread of rashes along the nerves.
In erysipelas, hyperemia and edema have clear sharply defined boundaries, accompanied by peripheral growth, absence of neuralgic pains and mandatory fever.
Herpes zoster: treatment
The earlier treatment began, the more effective it is.
Antiviral drugs are prescribed:
- valtrex three times a day for 1 g for 7 days;
- acyclovir( virolex, zovirax) five times a day for 800 mg inside for up to 10 days;
- famvir 3 times a day for 250 mg a week.
Local treatment:
- compliance with rational regimen( wash is prohibited, the skin around the lesion is wiped with 2% salicylic alcohol);
- use of local antiviral drugs, which are applied 4 times to the lesion site: ointment florenal, zovirax, megosin, tebrofen. And also symptomatic means - fukortsin, alcohol solutions of aniline dyes.
Pains diadynamic currents, acupuncture, combination of ultrasound and microwave irradiation, percutaneous neuroelectrostimulation contribute to pain relief.