Legionellosis pneumonia
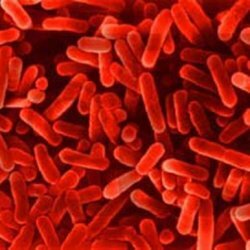 The intracellular legionella microbe refers to gram-negative( Gr -) bacteria. The stick itself is legionellosis up to 3 μm in size and is equipped with organoids of movement - flagella. The natural area of its habitat is fresh water. The human body for this pathogen appears to be a biological dead end, so infection is not transmitted from the individual to the individual. Legionellosis or legionellosis pneumonia is called a disease of legionnaires because of the case associated with its primary detection in 1976.
The intracellular legionella microbe refers to gram-negative( Gr -) bacteria. The stick itself is legionellosis up to 3 μm in size and is equipped with organoids of movement - flagella. The natural area of its habitat is fresh water. The human body for this pathogen appears to be a biological dead end, so infection is not transmitted from the individual to the individual. Legionellosis or legionellosis pneumonia is called a disease of legionnaires because of the case associated with its primary detection in 1976.
Legionellosis is being transferred:
1. Alimentarily:
- defective food;Poor metabolism.
2. Inhalation:
- through the respiratory system.
3. Sporadically:
- is seasonal, that is, from time to time.
Outbreaks of legionellosis pneumonia are possible with:
- Close proximity to open water bodies.
- By frequent visits to swimming pools.
- Presence in the air conditioner.
- Use of air humidifiers.
- System of forced ventilation.
Persons often exposed to disease:
- Workers on land.
- People with weak immunity.
- Persons who have reached the age of 40-60 years. For example, men are more likely to suffer from legionellosis than women. This ratio is 3/1.
Factors of importance for the development of Legionella wand:
- The presence of an aquatic environment for its habitat.
- Ponds with a lot of dirt and mud, especially stagnant with a water temperature of 20 ° -45 ° C.
- Mechanisms that promote the process of distribution of diasporas( dissemination):
- air conditioners;
- respiratory therapy.
4. Kind of bacteria and the necessary amount for the development of harmful products of the body( virulence).
People with a weakened immune system have quite a few microorganisms for the onset of the disease.
Clinical parameters of legionellosis:
- From pneumonia-free acute respiratory infections to severe pneumonia.
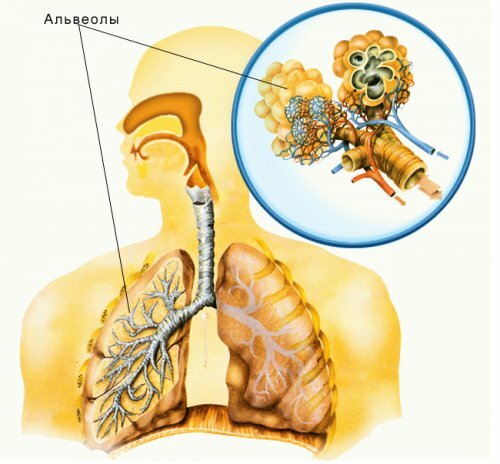
- Acute alveolitis with predominant dyspnea.
In most cases, legionellosis pneumonia occurs as a share, than for example as focal. The disease has an incubation period that can last from 2 to 10 days or 36 hours. In patients with weak immunity, the incubation period passes quickly. Symptoms during the incubation period:
- Drowsiness.
- Severe.
- Diffuse myalgia( pain in the muscles).
- Headache.
- Chills.
The further development of pneumonia is already expressed more sharply. It happens that some patients can not remember many moments from the first days of the disease.
Symptoms associated with acute form:
- High body temperature reaching 40 ° C.
- Severe intoxication.
- Headache.
- Mental status violation.
- Consciousness disorder with false perception( hallucinations).
- CNS( central nervous system) defeat.
- Chills with severe sweating.
- Persistent myalgia.
- Bradycardia( reduction of heartbeats).
Rare symptoms( from 20-50%) before fever in legionellosis:
- Diarrhea:
- pain spreading over the abdomen;
- nausea;
- vomiting;
- permanent diarrhea with characteristic sounds in the intestine.
- Cough.
- first moderate dry.
- further with sputum, in some cases even with purulent and bloody clots.
- Shortness of breath.
- During breathing, pain symptoms appear in the chest.
At the peak of fever in the blood, leukocytosis with a left shift to the left and increased ESR rates( up to 60 mm / h) and thrombocytopenia - that is, a decrease in blood platelets in the blood, often lead to excessive bleeding. In a laboratory study of urine, elevated leukocytes, protein and cylinders with erythrocytes in the sediment.
The clinical picture during the examination is more dependent on the lesions( seals) in an extensive form, that is, with radiological indices. However, dull sounds are also detected with percussion, weakened breathing, crepitation and wet wheezing.
Complications occurring in approximately 10-20%:
- Formation of a small pleural exudate( fluid in the pleural cavity).
- Unstable hemodynamics.
- Acute respiratory failure.
- Dysfunction of the digestive tract( digestive tract), as well as kidneys.
- Encephalopathy is a diffuse lesion of the brain.
X-ray of the lungs from the first time shows extensive seals or the formation of foci, some migrating infiltrates( a cluster of cellular components with high density and increased volume that are not characteristic of the body), which often occur in the right lower lobe, but also in two lungs at once.
Often there may be impairments during the initial etiotropic treatment with antibiotics, although the clinical indicators are quite positive. In severe cases of lethal inflammation, a pool of infiltration occurs that affects the segment or the entire lobe. In general, for this pneumonia, the disintegration of lung tissue is not typical.
The process of resorption of clusters( infiltration) takes a long time, sometimes several weeks. After that months, residual changes may remain until they are resolved at all. In many cases, scars on the lungs remain. Some patients, even after an absolute cure, complain for a long time about weakness and rapid fatigue.
Bronchiectasis( purulent-inflammatory destruction of the bronchial wall) or bronchial cancer slows the resolution of pneumonia, and does not contribute to the occurrence of relapses.
Complications, arising from legionellosis
1. Pulmonary:
- acute respiratory failure;
- cavity in the lung.
2. Extrapulmonary:
- gastrointestinal bleeding;
- vomiting;
- diarrhea;
- pancreatitis;
- paralytic ileus( intestinal obstruction);
- is an intestinal infection( local).
3. Enlargement of liver enzymes.
4. CNS lesion.
5. Kidney damage:
- hematuria;
- proteinuria;
- oliguria;
- acute renal failure;
- glomerulonephritis;
- interstitial nephritis.
6. Cardiovascular:
- shock with possible fatal outcome;
- pericarditis with sweating;
- myocarditis;
- endocarditis.
7. Musculoskeletal:
- myositis;
- arthropathy.
Treatment of legionella pneumonia
Although it is difficult to diagnose atypical pneumonia, they are treated exceptionally well and effectively. In the course of treatment, antibiotics with high lipophilicity are used, which easily penetrate the cell walls and create a high concentration within it capable of destroying all the pathogens of infectious pneumonia and, of course, Legionella.
Preparations for the treatment of legionellosis:
1. Medicines of the Macrolide groups:
- erythromycin;
- spiramycin:
- clarithromycin;
- azithromycin and the rest.
2. Tetracyclines:
- doxycycline;
3. Fluoroquinolones:
- ofloxacin;
- ciprofloxacin.
4. Rifampicin:
- macrolides with a weak alkaline reaction, as a more gentle option.
Macrolides are prescribed during a severe course of an infectious disease, initially as intravenous injections with high doses, and then orally. With easier flow, antibiotics are determined immediately in the form of tablets.
- Intravenous erythromycin up to 4 grams per day.
- Oral - erythromycin 250 mg;500 mg in 4 divided doses per day;
- clarithromycin 250 mg twice daily.
- Sometimes erythromycin is combined with rifampicin. They take antibiotics for 2 weeks. Azithromycin has the ability to accumulate in the body, so it is convenient to prescribe it with short courses of treatment.
Legionellosis pneumonia is a serious and serious disease, especially since it is very difficult to diagnose it. When the first symptoms of pneumonia appear, contact a doctor immediately and do not tighten.