Thyroid cancer - symptoms, risk factors
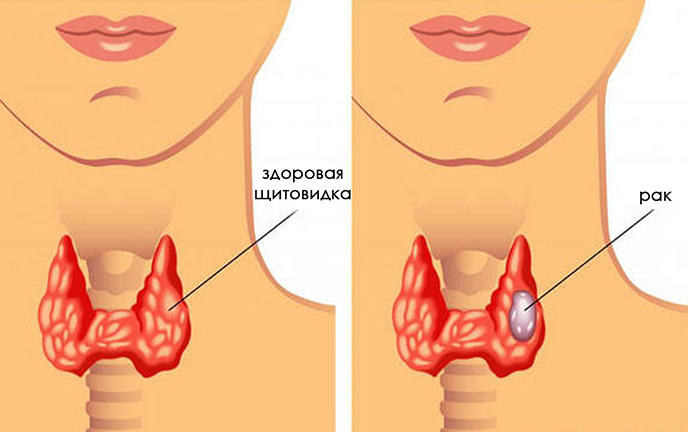
Oncology of the thyroid gland is a malignant neoplasm from the gland cells. The prognosis for the life and health of the patient with this disease depends on the histological picture, the stage of the process, the concomitant diseases.
Content
- 1 Statistics: incidence, prevalence,
- 2 mortality Symptoms
- 3 Risk Factors
- 4 classification of tumors
- 4.1 Papillary carcinoma
- 4.2 Follicular carcinoma
- 4.3 Medullary carcinoma
- 4.4 Anaplastic carcinoma
- 5 cancer metastases of thyroid
- 6 Diagnostics
- 7 Stage
- 7.1 Up to 45 years
- 7.2 After 45 years
- 8 Treatment and prognosis
Statistics: incidence, prevalence, cmThe incidence of
Of all newly diagnosed malignant tumors, thyroid cancer is only 0.5-1% of cases. Somewhat more often neoplasms of thyroid tissue are found in residents of regions with iodine deficiency. Most of the territory of our country belongs to such areas. Mortality from thyroid cancer is also high in the Mediterranean regions.
Oncology can be an accidental finding on autopsy. In such situations, a person dies for other reasons, and a tumor of thyroid tissue is first discovered on the pathoanatomical autopsy. It is known that in Japan the prevalence of such hidden cancer reaches 25-30%.In other countries it is lower. But, nevertheless, scientists agree that most cases of thyroid cancer are not diagnosed during life and is not the cause of death.
Oncology of thyroid tissue occurs in men and women. Representatives of the stronger sex fall ill 4 times less often. Cancer can occur at any age.
There are two peaks in incidence:
- 10-20 years( juvenile);
- 45-65 years( middle age).
The average age is up to 65-70% of all cases of pathology.
Every year, thyroid cancer is detected more often. A pronounced positive trend is observed in all population groups.
Mortality in thyroid cancer is relatively low. It accounts for less than 1% of all deaths due to malignant neoplasms.
Every 100,000 people die of this disease each year:
- 1 male;
- 2-3 women.
Symptoms of the disease
Diagnosis of thyroid cancer in the early stages is difficult due to the lack of a vivid clinical picture. The first signs of a tumor are similar to those of a benign node or adenoma. Only after some time there are complaints pointing to oncology.
There are 4 groups of symptoms( see Table 1):
- arising from a node in the gland;
- due to regional distribution;
- signs of metastases;
- nonspecific reactions from organs and systems.
Table 1 - Clinical manifestations of thyroid tumors.
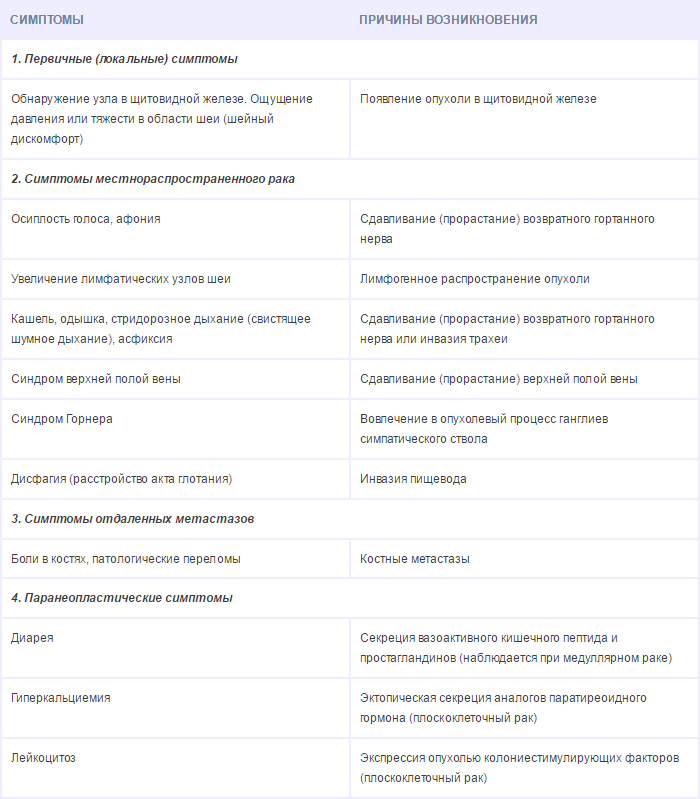
Primary focus can be of different sizes. Most often it can be determined by examination and palpation of the gland. The cancer node has a high density. This neoplasm is not uniform to the touch. Sometimes patients note the soreness of the knot. The primary focus of the tumor can grow rapidly in size. On average, for six months it increases in diameter by more than 5 mm.
Because of the germination of cancer in the surrounding tissue, there is a lesion of nerves, veins, and neck organs.
Patients are concerned:
- hoarseness of the voice;
- asphyxiation;
- swallowing disorder;
- widening of the veins on the chest.
Metastases in the cervical lymph nodes make them dense, painful, limited in mobility. Such lymph nodes are large( more than 2 cm in diameter).Paratracheal, anterior jugular, lateral cervical lymph nodes, mediastinal nodes are involved in the process.
Remote metastases manifest themselves as pain syndrome, pneumonia, pleurisy, multiple fractures, etc.
Risk Factors
All causes of thyroid cancer have not been studied so far. The most significant risks of cancer are associated with heredity and exposure to radiation.
Adverse factors:
- family forms of thyroid cancer;
- presence of nodular or mixed goiter without thyrotoxicosis;
- hormonal imbalance;
- deficiency in the diet of iodine, cobalt, selenium, copper;
- radioactive irradiation of the head and neck;
- radioisotope study with iodine-131;
- stay in the zone of nuclear accidents;
- chemotherapy;
- adverse environmental conditions( contamination with radionuclides).
Almost all diseases of the thyroid gland with hyperplasia can be considered precancerous. These states are classified as background, since their direct connection to cancer is not proven. But statistics confirms the existence of common causes for hyperplasia and malignant degeneration of thyroid tissue.
Background processes include:
- chronic autoimmune thyroiditis;
- nodular goiter;
- diffuse goiter;
- adenoma.
The most suspicious are the nodes of the thyroid gland. If there is only one focal formation in the tissue, the risk of its malignancy is higher.
Groups of people with the greatest likelihood of oncology:
- men of any age with focal formations;
- young people under 25 with nodular goiter;
- people older than 55-60 years with nodular goiter;
- women with chronic diseases of the mammary glands and genitals;
- patients exposed to radiation( especially at the age of 10-12 years);
- persons with recurrent endemic goiter.
Classification of neoplasms
Malignant thyroid tumors are classified according to the histological structure and prevalence of the process. Thyroid cancer is a tumor of epithelial origin.
Classification of epithelial cancers:
- papillary;
- follicular;
- is medullary;
- anaplastic.
Papillary carcinoma
The most commonly encountered papillary tumor. Its share reaches 75%.Men get sick less often( 6-7 times).The average age at the time of oncology debut is 40 years. The disease is relatively favorable. The prognosis for life is good. The pathology continues for a long time, since the process of spreading such a tumor is slow.
Papillary cancer usually has several primary foci( multiple rudiments).A tumor rarely metastasizes through the lymph and blood to distant organs. Regional metastases( metastases in the lymph nodes) are found in 35-50% of cases. Sometimes such foci of tumor spread are the first manifestations of cancer. Metastases can grow much faster than the primary focus.
Dimensions of the neoplasm with papillary cancer vary. So, in the case of sclerosing microcarcinoma, the primary focus has a microscopic diameter and is detected only with the help of optical equipment. In other situations, the carcinoma occupies the entire volume of the thyroid gland, and its diameter exceeds 4-10 cm.
The histological structure of the tumor is also diverse. Under the microscope, papillary formations with a cylindrical or cubic epithelium are found. In addition, follicular foci and solid fields, psammal bodies, can be found.
Solid fields are an unfavorable sign and indicate a heavier forecast.
Papillary cancer refers to highly differentiated and functionally active. His cells are capable of producing hormones. A special analysis( immunochemical study) in the overwhelming majority of cases demonstrates the presence of thyroglobulin in the tumor material.
Follicular carcinoma
Follicular tumor is detected in 9-14% of patients. Men get sick less often in 7-9 times. The average age of patients with this diagnosis is 47 years. The cancer spreads slowly. The prognosis for life is favorable.
Follicular cancer can metastasize to distant organs. The most common hematogenous pathway. Metastases are found in the bones, lungs. Local( regional) distribution is uncharacteristic.
During the analysis of the material, the histologist detects follicles and trabeculae. Also, solid fields can be found. Papillary( papillary) structures are not detected. Follicular cancer can germinate into arterial and venous vessels.
Tumor refers to functionally active and highly differentiated.
Medullary carcinoma
Medullary neoplasm arises from C-cells( parafollicular).It is diagnosed in 3-8% of cases. Men get sick 1,5 times less often than women. The average age of patients at the time of onset of the disease is 46 years.
Medullary cancer is quite aggressive. His cells synthesize calcitonin. Usually this hormone does not have a fundamental effect on the mineral metabolism. But the medullary tumor secretes an extremely large amount of calcitonin. Therefore, patients develop a characteristic clinical picture, including diarrhea.
In the early stages of the disease, regional metastases appear. The tumor extends to the lymph nodes of the neck. Later there are distant( in other organs and parts of the body) metastases.
Medullary cancer is not associated with exposure to iodine isotopes.
Unfavorable prognosis for this pathology:
- in men;
- in people older than 50-55 years;
- in the syndrome MEN-II-B;
- in the presence of distant metastases.
Medullary cancer can be associated with heredity.
Statistically:
- 20% of cases occur in genetic syndromes( MEN II, congenital cancer);
- 80% - sporadic forms.
Histologists detect foci of tumor cells in the medullary cancer, fibrotic stroma, amorphous amyloid.
Anaplastic carcinoma
Anaplastic cancer is an extremely aggressive tumor. The prognosis for this disease is unfavorable. Men are ill as often as women. The average age of patients is 50-60 years.
The tumor is characterized by regional( 50%) and distant( 20%) metastasis.
Thyroid gland metastases
Thyroid tumors can give both distant( in the bone system, lungs, liver, brain) and regional( in the closest to the outbreak lymph nodes) metastases. The most often distant foci of the tumor are found in the lungs.
Metastases in pulmonary tissue give:
- follicular cancers - 22%;
- papillary cancers - 8%;
- papillary-follicular cancers 17%;
- medullary cancers - 35%.
Foci can be multiple or single.
Metastases in bone tissue for all types of thyroid cancer - up to 14%.Foci of the tumor usually destroy the solid tissue of the skeleton( osteolytic type).Metastases are found more often in flat bones( ribs, pelvis, skull, spine, sternum).For a long time, foci are not detected on X-rays. The presence of metastasis can confirm a radioisotope study with iodine or technetium.
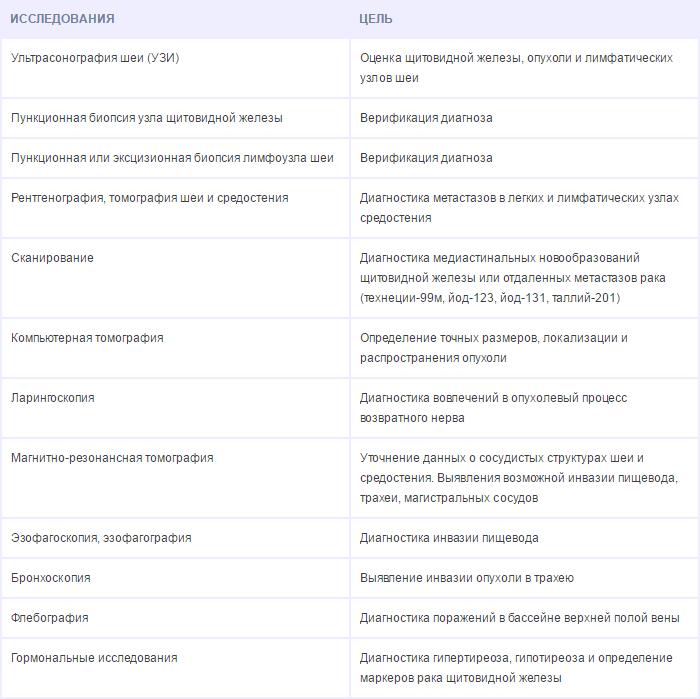
Diagnosis
Diagnosis of cancer in the early stages is the key to the most effective treatment. All programs for clinical examination of patients with nodular goiter and other diseases of the gland are directed, including, to the detection of oncology.
Early diagnosis is carried out:
- among people living in areas contaminated with radioactive iodine;
- among patients with hypothyroidism;
- in relatives of patients with medullary cancer.
Screening includes at least a patient's examination, anamnesis, palpation of the gland and ultrasound. In addition, it is desirable to determine the level of thyroid-stimulating hormone. In all patients with nodular goiter from risk groups, it is recommended to take an analysis for calcitonin.
To confirm the diagnosis apply:
- thyroid ultrasound;
- fine needle aspiration biopsy;
- scintigraphy;
- histological examination.
It is especially important to examine patients if focal education:
- is in an isthmus;
- has an active blood supply;
- is heterogeneous in structure;
- has fuzzy boundaries;
- contains calcification sites.
As a follow-up, a puncture is prescribed. This method of biopsy allows you to take material from the tumor into a cytology. By the results of the analysis, a diagnosis of cancer can be established. Puncture can not differentiate follicular adenoma and carcinoma. Also to the shortcomings of the method is its high sensitivity to the qualification of the doctor and compliance with the technology.
Scintigraphy with radioisotopes makes it possible to assess the presence of a node and its activity. Most thyroid tumors look like "cold" nodes. The main advantage of the technique is that it allows to detect metastases.
Histology during and after surgery is the most accurate diagnosis. Based on the results of this survey, the attending physician chooses further tactics.
Table 2 - Diagnostic studies for tumors of the thyroid gland.
Stages of
The prevalence of thyroid cancer is assessed by the clinical classification of TNM.
It takes into account:
- primary focus( T);
- metastasis in regional lymph nodes( N);
- distant metastases( M).
The primary focus is estimated from 0 to 4. In this case, T0 is diagnosed if the focus is not detected, T1 - in a tumor up to 2 cm, T2 - for a tumor of 2-4 cm, T3 for a tumor of 4 cm, and T4 for tumor growth inCapsule.
Regional lymph nodes are classified as N0( no lesions), N1( there are metastases in the lymph nodes of the neck).
The distant foci of the tumor in the TNM system are classified into 2 positions: M0( no metastasis) and M1( there are distant metastases).
The stages of thyroid gland malignancy are determined from histology data, taking into account the TNM classification and age of the patient.
Up to 45 years old
In young patients( up to 45 years old) with papillary and follicular cancer, one of 2 stages is established:
- Stage 1 - no distant metastases;
- Stage 2 - there are metastases.
After 45 years of
After 45 years in patients, one of the 4 stages can be established:
- 1 stage-T1, N0, M0;
- Stage 2 - T2, N0, M0;
- Stage 3 - T3, N0, M0 or T1-3, N1, M0;
- 4th stage - all the rest.
All cases of anaplastic cancer are classified into 4 stages.
Treatment and prognosis
Cancer treatment is complex. Usually, the tumor and metastases are removed surgically, then hormonal suppressive therapy is performed.
In cases of iodine-sensitive tumors, treatment may be radioisotope. The patient receives a pharmacological drug that destroys the primary focus and all metastases. The effectiveness is controlled by scintigraphy.
If the tumor is anaplastic, then it is removed surgically or exposed to high-intensity radiation.
Prognosis for papillary cancer:
- Stage 1 - survival rate of about 100%;
- Stage 2 - survival rate of about 100%;
- Stage 3 - 93%;
- Stage 4 - 50%.
Five-year survival rate for follicular cancer:
- Stage 1 - survival rate of about 100%;
- Stage 2 - survival rate of about 100%;
- Stage 3 - 70%;
- Stage 4 - 50%.
In follicular cancer, the prognosis is somewhat worse:
- Stage 1 - survival rate about 100%;
- 2nd stage - 98%;
- Stage 3 - 80%;
- Stage 4 - 30%.
All patients after radical treatment of thyroid cancer are on the account of an endocrinologist and an oncologist. To correct postoperative hypothyroidism and suppressive therapy, synthetic analogues of thyroxine and triiodothyronine are used.
Doctor-endocrinologist Tsvetkova IG
Recommended for viewing:



