Diagnosis of diabetes mellitus and classification
Diabetes mellitus( DM) is one of the most common non-infectious diseases. The negative consequences of diabetes for mankind are manifold. This pathology reduces the quality of life, increases mortality in young and middle age, takes away a significant part of health budgets in all countries of the world.
In Russia, the incidence rate is quite high. Only on request for medical care there are 4.04 million patients with diabetes. The results of epidemiological studies suggest that the true number of patients is even higher. Probably, about 7-10% of the population of our country has a violation of carbohydrate metabolism in an explicit or latent form.
Contents of
- 1 What is diabetes?
- 2 Diagnosis of hyperglycemia
- 2.1 Clinical features
- 2.2 Blood sugar examination
- 2.3 Glycemic hemoglobin
- 3 Classification of diabetes by types
- 4 Diabetes mellitus type 1: features, diagnostic principles
- 5 Diabetes mellitus type 2: classification and diagnosis
- 6 Differential diagnosis of diabetes mellitus 1-1st and 2nd type
- 7 Other types of diabetes
What is diabetes?
Diabetes mellitus is a number of different pathologies that combine one parameter - chronic hyperglycemia.
Excess blood sugar concentration can be associated with:
- decrease in insulin production in the body;
- decreased tissue sensitivity to insulin;
- combination of these factors.
Normally, glucose is a universal source of energy for all cells in the body. A person gets carbohydrates, fats and proteins from his food. All these components can be converted into glucose. First of all, sugar in the blood raises carbohydrates.
Blood delivers glucose to all organ systems. Inside most cells, this substance penetrates through a special hormone-mediator( insulin).Insulin binds to receptors on the surface of cells and opens up special channels for glucose.
This hormone is the only substance that lowers blood sugar levels. If the synthesis of insulin is blocked, then the cells stop absorbing glucose. Sugar accumulates in the blood, causing a cascade of pathological reactions.
Similar changes occur due to the improper functioning of the receptors for insulin. In this case, the hormone is produced, but the cells do not perceive it. The result of low sensitivity to insulin is chronic hyperglycemia and characteristic metabolic disorders.
Immediate Effects of Hyperglycemia:
- Enhanced Lipid Disintegration in Cells;
- decrease in blood pH;
- accumulation in the blood of ketone bodies;
- release of glucose in the urine;
- excess fluid loss with urine due to osmotic diuresis;
- dehydration;
- changes in electrolyte blood composition;
- glycosylation( damage) of the vascular wall proteins and other tissues.
Chronic hyperglycemia results in damage to almost all organs and systems. Particularly sensitive to violations of carbohydrate metabolism:
- kidney vessels;
- vessels of the fundus;
- crystalline lens;
- central nervous system;
- peripheral sensory and motor neurons;
- all major arteries;
- liver cells, etc.
Diagnosis of hyperglycemia
Clinical signs of
Diabetes can be detected by accident during a routine checkup or during a targeted examination.
Clinical signs of hyperglycemia:
- severe thirst;
- a constant sense of hunger;
- rapid urination;
- itching and dry skin;
- strong weakness.
In severe cases, when the patient has almost no own insulin, there is a pronounced decrease in body weight. The patient is losing weight even with a good appetite.
Blood sugar test
To confirm the diagnosis of diabetes it is necessary to reveal hyperglycemia.
For this, examine the blood sugar level:
- on an empty stomach;
- during the day;
- during an oral glucose tolerance test( OGTT).
Fasting glucose is a glycemia after 8-14 hours of complete abstinence from food and drinks( except drinking water).For greater accuracy, it is necessary to refrain from taking medications, smoking, using chewing gum, etc., before the analysis in the morning. In normal state, fasting sugar is 3.3-3.5 mM / l in capillary blood( Figure 1) and up to 6.1MM / l in venous plasma( Figure 2).
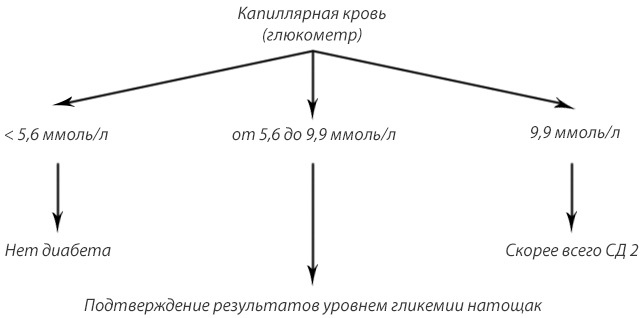
Fig.1 - Screening of DM 2 and impaired fasting glycemia by whole capillary blood.
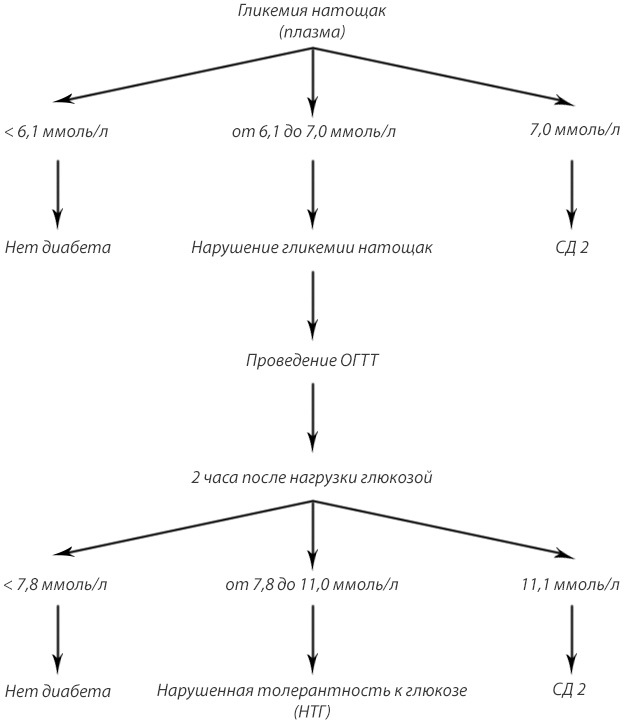
Fig.2 - Screening of DM 2 and other disorders of carbohydrate metabolism by plasma.
Glucose during the day - any random measurement of blood sugar. In a healthy person, the glycemia never exceeds 11.1 mM / l.
Oral glucose tolerance test( "sugar curve") is a sample with a load. The patient is taking blood on an empty stomach and after taking sweet water( 75 g of anhydrous glucose for 250-300 ml of water).Usually, glycemia is measured 2 hours after the load.
During the test, one should not eat, drink, actively move, take medicines, smoke, strongly worry. All these factors can affect the results of the study.
A glucose tolerance test can not be performed:
- if fasting sugar is more than 6.1 mM / l;
- during colds and other acute illnesses;
- during a short course of treatment with drugs that raise blood sugar.
The norm is sugar to 5.5 mM / l( capillary blood) before the load and up to 7.8 mM / L 2 hours after.
Diabetes mellitus is diagnosed if:
- is at least twice the result of 6.1 or more fasting;
- revealed at least a one-time excess of 11.1 mM / l at any time of day;
- during the test, fasting sugar is more than 6.1 mM / L, after the load - more than 11.1 mM / l.
Table 1 - Criteria for diagnosis of diabetes and other disorders of carbohydrate metabolism( WHO, 1999).
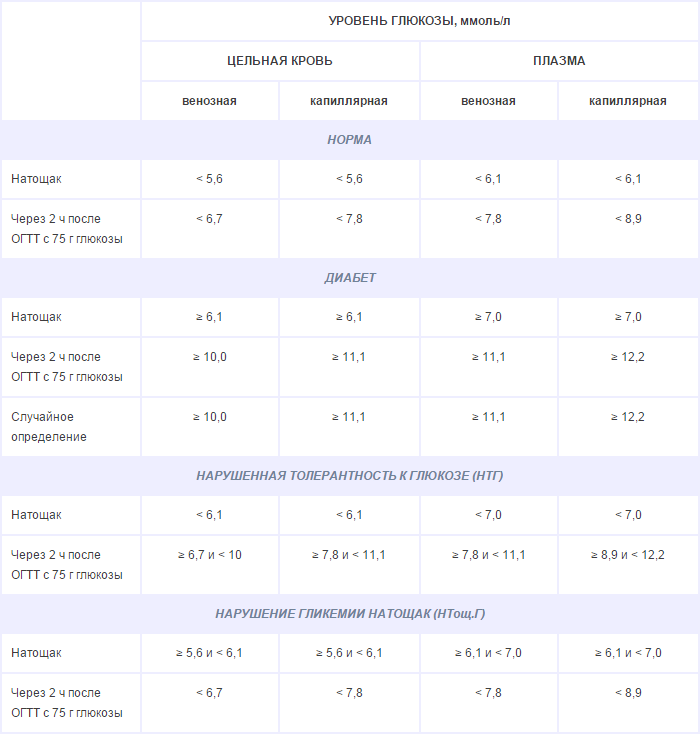
Using a glucose tolerance test, it is possible to detect the conditions of prediabetes:
- fasting hyperglycaemia( sugar before breakdown 5.6-6.0 mM / l, after loading - up to 7.8 mmol);
- impaired glucose tolerance( fasting sugar to 6.1 mM / L, after loading - from 7.9 to 11.0 mM / l).
Glycated hemoglobin
Recently, disorders in carbohydrate metabolism have been recommended to be diagnosed using glycated( glycosylated) hemoglobin. This analysis estimates the proportion of hemoglobin damaged by glucose. The higher the blood sugar in the last 3-4 months( the life span of the erythrocyte), the greater the proportion of glycated hemoglobin.
To diagnose diabetes, you need to get the level of this indicator more than 6.5%.The norm for glycated hemoglobin is 4-6%.The proportion of prediabetes is 6-6.5%.
If high levels of blood glucose or glycated hemoglobin are detected by chance, experts evaluate the clinical signs of hyperglycemia. Usually it is required to re-determine the blood sugar or conduct a stress test. Special samples are also used to establish the type of disease.
Classification of diabetes by types of
Hyperglycemia develops due to various factors. In 1999, the World Health Organization( WHO) developed a classification of diabetes mellitus, depending on the causes of its occurrence. This classification was further improved and supplemented.
Currently, there are 4 large types:
- type 1 diabetes mellitus;
- type 2 diabetes mellitus;
- other types of diabetes;
- gestational diabetes mellitus.
The greatest number of patients - patients with type 2 disease. They account for up to 90-95% of all cases. The next most common is type 1 diabetes. They suffer from about 4-9% of patients. All other forms on average account for about 1% of diabetic patients.
Boys get 1 type in childhood and adolescence somewhat more often than girls. The peak incidence is at the age of 7 and 14 years. After 30 years, cases of manifestation of the disease are quite rare.
Type 2 diabetes is 1.5-2 times less common in men than in women. Especially the difference in the groups of patients over 45 years is especially high. Currently, the incidence of type 2 diabetes at a young age is increasing dramatically. A decade ago, cases of this type in children and adolescents were casuistry. Now the disease is diagnosed in young people under 30 years with a frequency of 2-4 cases per 100,000 population. Diabetes type 2 is very often diagnosed late and its treatment is not given due importance. This is indicated by the high mortality rate of patients in the first years after the manifestation of the disease. So, within five years, up to a third of men and about a quarter of women die. Probably, many representatives of the stronger sex do not undergo the necessary examination and treatment, already having a diagnosis of type 2 diabetes.
Other rare types of diabetes mellitus are approximately equally common in men and women. An exception is pancreatogenic diabetes. In men, this form is detected more often and is usually associated with the abuse of alcoholic beverages and surrogates of alcohol. The share of women is up to 40%.They have pancreatogenic diabetes more often associated with the pathology of the biliary tract( cholecystitis, cholangitis).
Gestational diabetes - a violation of carbohydrate metabolism, first emerged during pregnancy. This diagnosis can not be established by a man for natural reasons. But the presence of gestational diabetes in the mother during pregnancy should be taken into account during the collection of anamnesis. If a man was born with a weight of more than 4-4.5 kg or his mother encountered impaired carbohydrate metabolism during pregnancy, then the risk of type 2 diabetes is significantly higher. This is due primarily to the burdened heredity of insulin resistance. On average, up to 50% of men with such an anamnesis develop type 2 diabetes after 40 years.
Type 1 diabetes mellitus: features, diagnostic principles
Type 1 diabetes mellitus is a disease in which the synthesis of your own insulin in the body is almost completely absent. The cause of this is the destruction of beta cells of the pancreas that produce the hormone. Type 1 diabetes mellitus is an autoimmune disease. Beta cells die due to an incorrect reaction of the body's defenses. Immunity for some reason takes endocrine cells for foreign ones and starts destroying them with antibodies.
To diagnose the disease you need:
- to assess the level of glycemia;
- to investigate glycated hemoglobin;
- determine the level of C-peptide and insulin;
- to identify antibodies( to beta cells, to insulin, to GAD / glutamate decarboxylase).
Type I is characterized by:
- chronic hyperglycemia;
- low level of C-peptide;
- low level of insulin;
- the presence of antibodies.
Diabetes mellitus type 2: classification and diagnosis
2 type of the disease develops because of the relative deficiency of insulin. The secretion of the hormone is always preserved. Therefore, metabolic shifts with this form of the disease are less pronounced( for example, ketosis and ketoacidosis practically never develop).
Type 2 diabetes mellitus is:
- mainly due to insulin resistance;
- mainly due to impaired secretion;
- mixed form.
For the diagnosis use an anamnesis, general examination and laboratory tests.
In the analyzes revealed:
- high blood sugar;
- elevated glycated hemoglobin;
- high or normal C-peptide;
- high or normal insulin;
- no antibodies.
Endocrinologists use special indices( HOMO, CARO) to confirm insulin resistance. They allow mathematically to prove the low sensitivity of tissues to their own hormone.
Differential diagnosis of type 1 and type 2 diabetes
Type 1 and type 2 diabetes mellitus has a common clinical picture and at the same time significant differences( see Table 2).
Table 2 - The main differential diagnostic signs of diabetes mellitus type 1 and type 2.

Other types of diabetes
Specific types of diabetes mellitus are a heterogeneous group that includes many subtypes of the disease.
Diabetes is distinguished due to:
- of genetic defects of beta-cell function( MODY-1-9, transient neonatal diabetes, permanent neonatal diabetes, mitochondrial DNA mutation);
- genetic defects of insulin action( insulin resistance type A, leprechaunism, Rabson-Mendenhall syndrome, lipoatrophic diabetes);
- pancreatic disease( pancreatitis, swelling, trauma, cystic fibrosis, etc.);
- of other endocrine diseases( thyrotoxicosis, hypercorticism, acromegaly, etc.);
- medicines and chemicals( the most common form is steroid);
- infections( congenital rubella, cytomegalovirus, etc.);
- unusual autoimmune reactions;
- of other genetic syndromes( syndromes of Turner, Wolfram, Down, Klinefelter, Lawrence-Moon-Biddle, porphyria, Huntington's chorea, Friedreich's ataxia, etc.);
- other reasons.
To diagnose these rare forms of the disease requires:
- anamnesis;
- evaluation of hereditary burden;
- genetic analysis;
- study of glycemia, glycated hemoglobin, insulin, C-peptide, antibodies;
- definition of a number of biochemical indicators of blood and hormones;
- additional instrumental studies( ultrasound, tomography, etc.)
Rare forms of diabetes require great diagnostic capabilities. If the conditions are limited, then it is important to reveal not the cause of the disease and its exact type, but the degree of insulin deficiency. The further tactics of treatment depend on this.
Doctor-endocrinologist Tsvetkova IG
Recommended for viewing: