Vagotomy with a stomach ulcer
Vagotomy is an operation that involves the intersection of a vagus nerve or part of it. This operation began to be applied from the forties of the last century, and the first operations at that time were conducted on animals. In 1967, this procedure was performed in the clinic, where in addition to vagotomy, pyloroplasty was performed-the evacuation of contents from the stomach. Now vagotomy is widely used in the treatment of gastric ulcer and other diseases of the gastrointestinal tract.
Vagotomy can be performed in three ways:
- Stem vagotomy, which is the intersection of the vagus nerve above or below the diaphragm, which allows you to actuate not only the stomach, but also other abdominal organs such as the intestine, liver, biliary tract and pancreas.
- Selective vagotomy, which is performed to cross all vagus nerves related to the stomach, and retains the vagus nerves that go to the liver, pancreas and intestines. This kind of vagotomy is practiced quite rarely, which is associated with one drawback: among the vagus nerves of the liver, intestine or pancreas, branches of the nerves of the stomach can pass.
- Proximal selective gastric vagotomy is an operation to partially intersect the vagus nerves of the stomach, that is, only the desired parts of the stomach are cleared. With gastric ulcer, this type of vagotomy has long been used in all countries of the world.
Vagotomy for stomach ulcers requires special anatomical knowledge from the operating physician in the work of the esophagus and gastrointestinal tract. This type of operation is considered much more complicated than the stem and selective vagotomy.
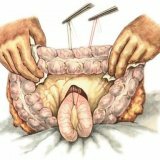
Places of intersection of the vagus nerve.
Consider the intersections of the vagus nerve with proximal gastric vagotomy. The anterior vagus nerve is located along the abdominal section of the esophagus, after which it passes into the gastro-hepatic ligament. A posterior vagal nerve passes along the posterior wall of the abdominal esophagus and, like the anterior vagus nerve, enters the gastro-hepatic ligament. It ends at the back of the antrum.
Abdominal incision occurs as in stem and selective vagotomy. The assistant must pull the large curvature with both hands down and to the left. Assistant specialist performs traction, which allows to detect the anterior vagus nerve, which has the form of a white strand, located along the length of the gastrohepatic ligament. The Latarjet nerve in some cases may have four terminal branches extending to the anterior wall of the antrum of the stomach, slightly below the small curvature of the stomach and is a crow's foot.
There are times when it is very difficult to find the Latarjet nerve. The branches of this nerve should be crossed slightly above the crow's foot so as not to cause a malfunction in the antrum section. In the avascular zone, you should carefully cut the gastrohepatic ligament with scissors, then stick your index finger and perform traction of the gastro-hepatic ligament, thereby separating the Latarjet nerve from the ligament, pushing it away from the small curvature of the stomach.
Instead of the method where the gastro-hepatic ligament is traced by the index finger, another method can be used, which in some cases is even more effective. The gastro-hepatic ligament is dissected as well as in the above-described method, after which the index and middle fingers are inserted into the hole. A soft curved clamp is inserted between the edge of the curvature above the terminal branches. Further, helping fingers, he gets into a small stuffing box.
Next, the end of the curved soft clamp is removed through the gastro-hepatic ligament, after which a thin tube is caught. After it should be carried out in the opposite direction and output through a small hole near the edge of small curvature. Its end is taken by a clamp, separated to the right and performs a traction, as a result of which the necessary Latarjet nerve is separated. This method somewhat facilitates bandaging and crossing of branches.
Stitches are superimposed on the small curvature of the stomach. This is done in order to prevent the occurrence of hematomas until the development of necrosis and other complications in the postoperative period.
To prevent the occurrence of a defect between the gastrohepatic ligament and small curvature, the ligament is sewn to a small curvature, while ensuring that nerves or branches do not enter the seam.
In the event that vagotomy, carried out with a stomach ulcer, failed, many specialists associate this with incomplete crossing of the vagus nerve. But in the case of a delay in evacuating the contents from the stomach due to an ineffective drainage operation, there may be an increase in gastric secretion, whereupon the ulcer does not heal or progress.
During the selection and trunk vagotomy, drainage operations are used: pyloroplasty and gastroduodenostomy.
The first method has some advantages over the second, namely:
- Properly performing this operation will provide excellent gastric drainage.
- This method is much easier than the second.
- This procedure maintains the gastric integrity, not permitting the confusion of duodenal, pancreatic and bile secrets with food.
- This method allows the examiner to examine the ulcer, reveal its degree and size, and also provides an opportunity to examine the gastric mucosa.
- If the ulcer is bleeding, it makes it possible to identify the place of bleeding and put seams there.
Vagotomy with duodenal ulcer or stomach ulcer is a very effective operation, which, if performed in a qualitative way, can save the patient from probable postoperative consequences.