Emakakaela erütroplastik
 Erythroplasty of the cervix is a change in the normal structure of the epithelium covering the cervix in the form of its atrophy of unknown origin. Erythroplasty is not diagnosed infrequently, which does not allow to study this pathology in sufficient detail, therefore it still remains poorly understood.
Erythroplasty of the cervix is a change in the normal structure of the epithelium covering the cervix in the form of its atrophy of unknown origin. Erythroplasty is not diagnosed infrequently, which does not allow to study this pathology in sufficient detail, therefore it still remains poorly understood.
Erythroplasty on the cervix affects that part of its surface that is well visualized in the vaginal cavity during a traditional gynecological examination. This part of the cervix is closely connected with the vaginal cavity not only anatomically, but also functionally. The epithelium covering the vagina and cervix has a single structure - it is represented by several layers of flat-shaped cells( multilayered flat), depends on the cyclic hormonal oscillations, has the ability to self-renew and solves the most important task - to protect the sexual way from unwanted infectious aggression.
The epithelium covering the cervix from the side of the vagina is called exocervix. The layers of the flat epithelium of exocervix are unequal in structure, since they perform different tasks. The mucous cervix has four layers, beneath it is a dense stromal structure - the basal membrane.
The lowest layer of epithelial cells is located on this membrane and is therefore called basal. There are many receptors( small nerve endings) that react sensitively to hormonal changes in the body.
Above the basal there is a second, parabasal, layer of epithelial cells, which have a high capacity for regeneration( recovery).The parabasal layer serves as a source of new cells.
The third, intermediate, layer of multilayer flat epithelium is formed as "young", newly formed, and "aging" cells.
The most superficial, fourth, layer of cells is in a state of constant renewal. His old cells are slouched and replenished with new ones formed in the lower layers.
The inside of the cervical canal mucosa has a different structure from the vaginal epithelium and is represented by a single layer of epithelial cells, similar to cylinders( cylindrical epithelium) of various sizes. These cylindrical cells adjoin each other loosely, forming intercellular grooves and crevices that perform the function of cervical glands( pseudo-iron) and produce a mucous secret. The mucosa located inside the cervical canal is called endocervix. Epithelium of endocervix is also located on the basement membrane and has its own reserve layer of cells for self-renewal.
On the surface of the cervix, there is a physiological opening opening the access to the cervical canal, called cervical( from the Greek "cervix" - neck or cervical).Where it connects to the vaginal cavity, there is a natural constriction, formed by a dense connective tissue - the external pharynx, which functions as a kind of "damper" capable of closing and opening the cervical cavity.
In the area of the external throat, a transitional zone( or a transformation zone) is localized, where the epithelium of the cervical surface connects with the epithelium of the cervical cavity.
Erythroplasty of the cervix is formed in the exocervical area, affecting a multilayered flat epithelium located around the outer throat. For some unknown reason, the multilayered epithelium begins to thin out in a delimited area, it loses its multilayeredness, that is, its atrophy develops.
There are no specific symptoms of erythroplasty of the cervix, but it is easy enough to diagnose it visually, since the mucosa area becomes thinner and begins to differ from the healthy surrounding epithelium. Complete the diagnosis of colposcopy, cytological and histological studies.
Treatment of erythroplasty of the cervix involves the removal of a pathological focus. All methods available in the arsenal of modern medicine are aimed at destroying( destroying) the site of atrophy and in most cases coincide with the methods of surgical treatment of pseudo-erosions.
Causes of erythroplasty of the cervix
Despite the unclear reasons for the appearance of erythroplasty on the neck, the most vulnerable groups of patients are identified for this pathology.
Since in patients erythroplasty is often associated with an infectious and inflammatory process, cervicitis and colpitis of various etiologies are regarded as one of the provoking factors for the development of erythroplasty of the cervix.
Structural disorders in the epithelium of exocervix inherent in erythroplasty can also cause trauma and damage to the cervical tissues of a mechanical or chemical origin. These include abortion, significant tissue damage in childbirth, diagnostic and therapeutic instrumental manipulation, the use of aggressive chemical compounds( for example, spermicide or improper means for douching).It is assumed that in cases of disturbances in the processes of regeneration( restoration) in the damaged neck tissues, erythroplasty can form.
Cervical tissues are structurally and functionally dependent on hormonal function and the state of the immune system. Expressed hormonal dysfunction and endocrine disorders are considered risk factors for the formation of erythroplasty of the cervix. The most significant is estrogenic insufficiency, which leads to disruption of the formation of new epithelial cells.
The role of the hereditary factor in the development of erythroplasty is discussed, as some patients in the family already have a similar pathology.
It should be noted that these conditions can be attributed to the provoking factors of erythroplasty of the cervix only conditionally, since infectious inflammation, hormonal and immune disorders are very common, and erythroplasty on their background is diagnosed extremely rarely.
Symptoms and signs of erythroplasty
Erythroplasty of the cervix is asymptomatic. Sometimes patients may notice minor, not associated with menstruation bloody discharge, since the severely thinning cervical epithelium is easily damaged. Flowing against the background of local infectious inflammation erythroplasty is accompanied by typical inflammatory manifestations, when patients complain of profuse purulent or serous-purulent leucorrhoea, discomfort and pain in the vaginal area.
When examining the cervix on its surface, clearly visible areas of the mucosa, painted in a bright red color, with uneven contours. The healthy mucous membrane of the cervix has a pale pink hue, since it has several layers. With erythroplasty, individual parts of the cervical epithelium become thinner, therefore the underlying structures and blood vessels are visible through them, so that the color of the pathological focus changes. Such foci look shiny and relatively easily begin to bleed when they come into contact with the instruments or during palpation.
Like any "suspicious" site on the mucous membrane of the cervix, detected during routine examination, erythroplasty requires a more detailed examination. For this purpose, colposcopic examination is always performed. Erythroplasty of the cervix is presented in the form of different in size and color( from pink to burgundy and even bluish) areas with clearly defined, but uneven borders. The surface of such foci is much thinner, resembling a thin, glossy film through which the underlying tissues show through. The thinned epithelium may have signs of keratinization( dyskeratosis).
During colposcopy a sample with 3% acetic acid solution and Lugol solution is carried out. After contact with acetic acid, the erythroplasty zone turns pale, and Lugol's solution does not change its color. These samples help differentiate erythroplasty of the cervix with other pathologies: ectopia, leukoplakia and others.
With erythroplasty of the cervix, the surface and intermediate layers become very thin, and the underlying basal and parabasal layers, on the contrary, expand( hypertrophy).Excessive proliferation of immature "young" cells can trigger the appearance of cells that are atypical for this part of the mucous structure, that is, with manifestations of atypia. The presence of atypical cells in small amounts is not dangerous, but if there are many of them, the probability of the onset of a malignant process arises, therefore erythroplasty always requires a more detailed study of the cellular composition and the state of surrounding tissues with the help of cytological and histological studies. Microscopic examination reveals a flattening of the integument epithelium and its atrophy, expansion and fullness of small vessels, proliferation( sometimes atypical hyperplasia) of cells of the basal layer. Surface cells can have signs of keratinization.
When a combination of erythroplasty of the cervix with the inflammatory process, an additional laboratory examination( crops, smears) of the microbial composition of the vaginal discharge and cervical canal is performed.
Treatment of erythroplasty of the cervix
Since erythroplasty of the cervix is often formed against the background of inflammation, before its treatment it is necessary to detect and eliminate the infection. The treatment is conducted according to the results of a laboratory test, which not only confirms the presence of an infectious inflammation and identifies the pathogen, but also determines the necessary antibiotics for its elimination. Antibiotic therapy can be carried out in the form of topical treatment, and systemic antibiotics are used if the infection is localized not only in the superficial epithelium, but also in the underlying structures. In addition to antibacterial therapy, anti-inflammatory and immunostimulating treatment is prescribed.
It is also necessary to pay attention to the hormonal status of the patient with erythroplasty. Expressed hormonal dysfunction creates an additional negative effect on the cervical epithelium and can complicate the healing process, so it needs to be adjusted.
Erythroplasty of the cervix to reverse development is not capable, therefore it must be eliminated by any of the known methods. All of them are aimed at destroying the pathological focus, so that in its place a normal multilayered epithelium is formed. Since the principle of treatment of erythroplasty is similar to that of pseudo-erosion of the cervix, the techniques used coincide.
Are used:
- Diathermocoagulation: moxibustion of tissues through high frequency currents. After the procedure, a small scab( scab) remains on the neck, and beneath it is a wound surface that gradually heals. When the wound completely heals, the scab is torn off, exposing a healthy mucous membrane. The method is one of the oldest, but it has not lost its relevance due to high efficiency( 98%).A significant disadvantage of "cauterization" is a small scar formed on the cervix, which can become a source of rupture of the cervical tissues in subsequent births.
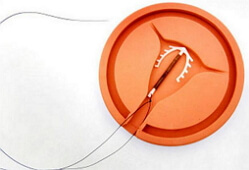
- Cryodestruction: destruction of the undesirable part of the cervical epithelium by deep freezing with liquid nitrogen. In fact, the method is similar to moxibustion, but it is less traumatic and there are no cicatricial changes on the cervix.
- Destruction of erythroplasty of the cervix by laser( laser-polarization).Laser radiation can evaporate the liquid contained in the cells, that is, unwanted cells literally evaporate, leaving only a healthy tissue on the neck.
- Radio wave therapy. A new technique based on the ability of radio waves to contactlessly "heat" cells to such a state that they are destroyed from within.
More aggressive surgical techniques are used when there are prerequisites for the oncology process.