Hemophilia: what is it, causes, symptoms, treatment, prognosis
Content
- What is hemophilia?
- What causes hemophilia?
- Symptoms and Signs
- Diagnostics
- Treatment
- Complications
- Can hemophilia be prevented?
- Forecast
What is hemophilia?
Hemophilia Is not one disease, but one of a group of inherited bleeding disorders that cause abnormal or excessive bleeding and poor blood clotting. The term is most commonly used to refer to two specific conditions known as hemophilia A and hemophilia B, which will be the main subjects of this article. Hemophilia A and B differ in a specific gene that mutates and encodes a defective clotting factor (protein) in each disease. Haemophilia C (factor XI deficiency) is rare, but its effect on clotting is much less pronounced than in A or B.
Hemophilia A and B are inherited in an X-linked recessive genetic pattern and are therefore much more common in men. This type of inheritance means that a given gene on the X chromosome is expressed only when there is no normal gene. For example, a boy has only one X chromosome, so the defective gene will be on his only X chromosome. Hemophilia is the most common X-linked genetic disorder.
Although much less common, a girl may also have hemophilia, but she must have a defective gene on both of her X chromosomes or one hemophilia gene plus a lost or defective copy of a second X chromosome that is supposed to carry normal genes. If a girl has one copy of a defective gene on one of her X chromosomes and a normal second X chromosome, she does not have hemophilia, but she is said to be heterozygous for hemophilia (i.e. e. is a carrier). Her male children have a 50% chance of inheriting one mutant X gene and thus have a 50% chance of inheriting hemophilia from the carrier mother.
Hemophilia A occurs in approximately 1 out of every 5000 live-born men. Hemophilia A and B occurs in all racial groups. Hemophilia A is about four times more common than hemophilia B. B occurs in about 1 in 20-30,000 live-born men.
Hemophilia is called the royal disease because Queen Victoria, Queen of England from 1837 to 1901, was the carrier of the disease. Her daughters passed on the mutated gene to members of the royal families of Germany, Spain and Russia. Alexandra, the granddaughter of Queen Victoria who became Tsarina of Russia in the early 20th century when she married Tsar Nicholas II, was a bearer. Their son, Tsarevich Alexei, suffered from hemophilia.
What causes hemophilia?
As mentioned above, hemophilia is caused by a genetic mutation. Mutations include genes that code for proteins required in the blood clotting process. Bleeding symptoms occur due to a bleeding disorder.
Read also:Multiple myeloma: what it is, why it occurs, what provokes the disease, symptoms and treatment
The blood clotting process involves a number of complex mechanisms involving 13 different proteins, classically called factors I through XIII and written in Roman numerals. If the lining of the blood vessels is damaged, platelets (blood elements) collect in the damaged area to form an initial plug. These activated platelets release chemicals that trigger the clotting cascade by activating a series of 13 proteins known as clotting factors. Ultimately, fibrin is formed, a protein that crosslinks with itself to form the mesh that makes up the final blood clot. The protein associated with hemophilia type A is factor VIII (factor 8) and with hemophilia type B it is factor IX (factor 9).
Hemophilia A is caused by a mutation in the factor VIII gene, so there is a deficiency of this clotting factor. Hemophilia B (also called Christmas disease) results from a factor IX deficiency due to a mutation in the corresponding gene.
A condition called hemophilia C involves a deficiency in clotting factor XI. This condition is much less common than hemophilia A and B and usually results in mild symptoms. It is also not inherited in an X-pattern and affects both sexes.
Hemophilia A is more common than hemophilia B. About 80% of people with hemophilia have type A hemophilia. Type B hemophilia occurs in about 1 in every 20,000–30,000 people. The subgroup of people with hemophilia B has the so-called Leiden phenotype, characterized by severe hemophilia in childhood that improves during puberty.
Symptoms and Signs

The disease can vary in severity, depending on the specific type of mutation (genetic defect). The degree of symptoms depends on the level of the clotting factor affected. Severe illness is defined as factor activity <1%, factor activity from 1% to 5% - a disease of moderate severity, and factor activity more than 5% - mild illness. The degree of bleeding depends on the severity (amount of factor activity) and is similar for hemophilia A and B.
In severe hemophilia (A or B), bleeding begins early in life and can occur spontaneously. Patients with mild hemophilia can only bleed in response to an injury or cut.
In severe disease, bleeding episodes usually begin within the first 2 years of life. Heavy bleeding after circumcision in men, it is sometimes the first sign of the disease. Symptoms may develop later in people with moderate to mild illness. Bleeding with hemophilia can occur anywhere in the body. Common sites for bleeding are joints, muscles, and the gastrointestinal tract.
Read also:Werlhof's disease (idiopathic thrombocytopenic purpura)
Specific sites and types of bleeding:
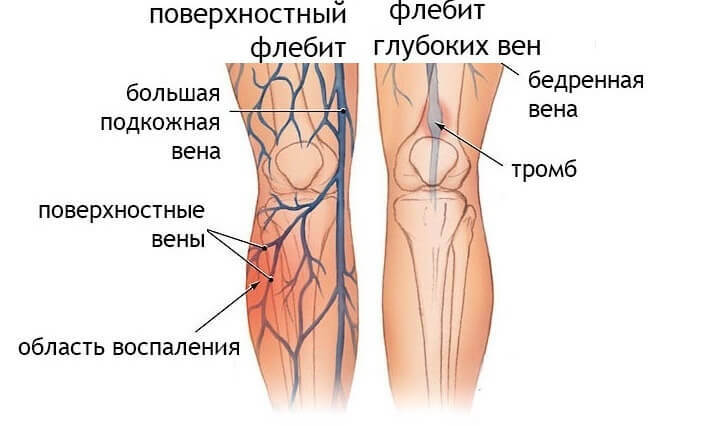
- Hemarthrosis (hemorrhage in the joint cavity) - The knees and ankles are most often affected. Bleeding causes stretching of the joint spaces, significant pain and, over time, can lead to disfigurement. Over time, joint destruction occurs and joint replacement surgeries may be required.
- Muscle bleeding with formation hematomas (compartment syndrome).
- Bleeding from the mouth or nose is possible. Bleeding after dental procedures and teething is common in young children.
- Bleeding from the gastrointestinal tract can lead to blood in stool.
- Bleeding from the urinary tract can lead to blood in urine (hematuria).
- Intracranial hemorrhage (bleeding into the brain or skull) can cause symptoms such as nausea, vomiting and / or lethargy and can be fatal.
- Excessive bleeding after surgery or injury.
Diagnostics
Most patients with hemophilia have a known family history of the condition. However, about one third of cases occur in the absence of a known family history. Most of these cases with no family history arise from a spontaneous mutation in the affected gene. Other cases may involve the affected gene passing through a long line of female carriers.
If a family history of hemophilia is unknown, blood test series can determine which part or factor of a protein in the blood clotting mechanism is defective if a person has abnormal bleeding.
The number of platelets (blood particles required for the clotting process) and bleeding time should be measured, as well as two indicators of blood clotting: prothrombin time (PTV) and activated partial thromboplastin time (APTT). For hemophilia A and B types, normal platelet and PTT counts and prolonged APTT are characteristic. Specific clotting factor tests can then be done to measure levels of factor VII or factor IX and confirm the diagnosis.
Genetic testing to identify and characterize specific mutations responsible for hemophilia is also available in specialized laboratories.
Treatment
The mainstay of treatment is the replacement of clotting factors. Clotting factor concentrates can be purified from human donated blood or manufactured in a laboratory using non-donated methods. This type of therapy is known as replacement therapy. Clotting factor replacement therapy is performed by injecting clotting factor concentrates into a vein, similar to a blood transfusion. This type of therapy can be done at home with proper instruction and training.
Read also:Thalassemia
Depending on the severity of the condition, replacement therapy for insufficient clotting factor can be performed as needed (called on-demand therapy) or regularly to prevent bleeding episodes (called prophylactic therapy).
People with mild cases of hemophilia A are sometimes treated with a drug desmopressin. This drug stimulates the release of substances from platelets that help form a clot from platelets. It is given either slowly intravenously or sometimes in the form of a nasal spray.
May be prescribed to relieve symptoms pain relievershowever, pain relievers other than aspirin or non-steroidal anti-inflammatory drugs (such as naproxen, ibuprofen), as these types of drugs additionally inhibit the blood's ability to clot. Acetaminophen (Tylenol, etc.) is often prescribed to relieve pain.
Complications

Bloodborne infections such as the HIV virus and hepatitis B and C, were a major complication of hemophilia treatment during the 1980s. These infections were transmitted through factor concentrates and other drugs that were used to treat hemophilia. The use of large pools of blood donors for the preparation of factor concentrates and the lack of special tests for infectious agents contributed to the contamination of blood products used for treatment hemophilia.
By 1985, about 90% of people with severe hemophilia were infected with the HIV virus, and about half of all people with hemophilia were HIV positive. Today, improved screening and manufacturing techniques, including virus removal techniques, as well as the development of recombinant factors, essentially eliminate this tragic complication of treatment.
Can hemophilia be prevented?
Hemophilia is a genetic (inherited) condition and cannot be prevented. Genetic counseling, carrier identification through molecular genetic testing, and prenatal diagnosis are available to help people understand the risk of having a baby with hemophilia.
Forecast
Prior to the development of factor concentrates, life expectancy in hemophilia patients was significantly reduced. Life expectancy until the 1960s for people with severe hemophilia was limited to 11 years. Currently, the mortality rate among men with hemophilia is twice that of healthy men. As mentioned earlier, the rise in therapy-related HIV and hepatitis infections during the 1980s led to a corresponding increase in mortality rates.
Currently, prompt and adequate treatment can significantly reduce the risk of life-threatening bleeding episodes and the severity of long-term joint damage, but deterioration of the joint condition remains a chronic complication of this disease.