Perioral dermatitis: symptoms, treatment regimen, prognosis
Content
- general information
- Causes and risk factors
- Risk factors:
- Signs and symptoms
- Diagnostics
- Treatment regimen
- Forecast
general information
Perioral dermatitis (PD) is chronic papular-pustular inflammation of the face, which is more common in women and children. Although the name suggests an eczematous disorder, it is clinically similar to acne or rosacea-like rash, with or without signs of mild eczema.
The mechanism of the onset and development of the disease has not yet been studied, since there are both internal and external factors. Many causes of perioral dermatitis have been proposed, from exposure topical corticosteroids before fluorine in water or toothpaste, but the etiology (cause) remains unknown.
Despite the name, perioral dermatitis is not true dermatitis. It mainly affects women of childbearing age and children, and the rash usually begins in nasolabial folds and spreads periorally, avoiding the area around the cinnabar lips (i.e. lip contour). It can also spread to the eyes or to the forehead.
Diagnosis is mainly clinical, depending on the appearance of a rash. Perioral dermatitis differs from acne lack of comedones. A biopsy is generally not required as there are several additional diagnostic tests that can draw attention to risk factors associated with trigger, as well as to frequent relapses of perioral dermatitis (microscopic examination for demodex, gastric acidity testing, positive testing for Helicobacter pylori).
The first step in improving PD is prevention by eliminating risk factors. The condition may improve in a few weeks. Although perioral dermatitis can be resolved in time after discontinuation of local corticosteroids and elimination of local irritants. The main therapeutic options are anti-inflammatory drugs and topical or systemic antibiotics. In severe cases, treatment may consist of topical corticosteroids, with gradual a decrease in the frequency of use and the subsequent transition to a therapeutic class with a lower efficiency. Perioral dermatitis is inflammatory skin disease with a chronic course and relapses.
Read also:Neurodermatitis: symptoms and treatment
Causes and risk factors

Perioral dermatitis is a clinically pronounced human skin reaction, mainly diagnosed in young women. Patients frequently report abuse of cosmetics and corticosteroid ointments. Although women with constitutionally dry skin or a history of atopic dermatitis mild forms suffer from this disease, inadequate use of local corticosteroids and intolerance to certain cosmetics may be associated with the pathogenesis of the disease.
The exact etiology of perioral dermatitis is not known. However, this disease occurs mainly in people with phototype I-II skin who have used creams with potent corticosteroids for a long time. Topical application of corticosteroids for various minor facial diseases often precedes the manifestations of perioral dermatitis. The inflammatory condition is limited to the skin only.
Risk factors:
- medicines - abuse of topical corticosteroids, inhalers or nasal medications is the main factor encountered risk, but no clear correlation between the risk of perioral dermatitis and drug efficacy or duration use;
- cosmetical tools - fluoride toothpaste, ointments and occlusive creams, especially those containing paraffin or petroleum jelly; Recently, sunscreens (SPF creams) have been identified as the cause of perioral dermatitis in children;
- physical factors: ultraviolet radiation, heat and cold intensify the eruption of the disease;
- microbiological factors: spindle-shaped bacilli, a microscopic parasite, were grown from perioral lesions in the laboratory Demodex folliculorum, views Candida (candida) and other mushrooms; their presence does not yet have a clear clinical significance, however oral candidiasis is a compromise factor in the occurrence of perioral dermatitis;
- other risk factors: hormonal factors (suspected as a result of exacerbation of premenstrual rash); oral contraceptives; gastrointestinal disorders such as infection Helicobacter pylori,gastritis, constipation, intestinal malabsorption.
Perioral dermatitis usually aggravated in the following situations:
- cleansing the face with unsuitable means, using soap, aggressive mechanical or chemical peels;
- some remedies against acne May cause or worsen a rash
- frequent use of creams on the affected areas (sunscreens, anti-wrinkle products, moisturizers, detergents skin care products), most of these skin care products contain ingredients that cause or enhance rash; anti-wrinkle and anti-aging products contain retinol, citric acid, beta and alpha hydroxy acids, which irritate and increase facial erythema;
- the use of topical steroids; the activity of steroids contained in the product used is directly proportional to the severity and rate of eruption of the rash;
- balms and lipsticks that extend beyond the lips can aggravate the condition.
Read also:Red spots on the human body: the causes of what diseases
Signs and symptoms

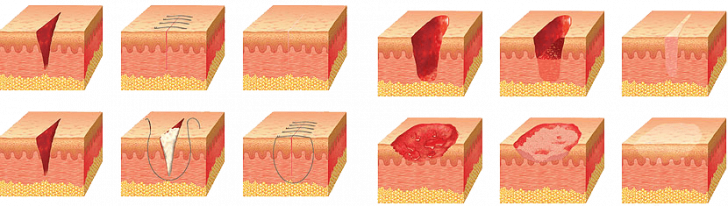
Perioral dermatitis is characterized by papulopustular rash and inflammatory erythema around the nose and mouth, chin, periocular region, and forehead. Papules and pustules are small and different from acne. photo above). Lesions appear as erythematous papules grouped follicularly, papulovesicles and papulopustules, or erythematous. The main distribution is perioral. The presence of closed or open comedones is not observed. Sometimes this is due to skin redness and local burning. Itching is rare. The condition tends to be chronic with periods of remission and relapse.
In the extreme, the state is called granulomatous perioral dermatitis, dermoscopy shows a yellowish appearance, defined by granulomatous infiltration. The lesions coalesce to form a plate bounded by the nasolabial folds and the chin.
Diagnostics
There are no laboratory tests that clearly define the disease. The following studies can help with diagnosis:
- serological testing for asymptomatic Helicobacter pylori infection;
- mycological research;
- isolating a growing population Demodex folliculorum;
- examination of stool samples to isolate malabsorption.
Zthe disease is similar to rosacea, but with less severe actinic damage to the skin and varies with the age of the patient. It can secrete lymphohistiocytic infiltrate with peripheral localization at all stages of the disease. Marked and sometimes granulomatous inflammation may be present, peripheral abscesseswhen pustules and papules are the dominant clinical presentation.
Differential diagnosis should be carried out with the following skin conditions: rosacea, acne vulgaris (acne), seborrheic dermatitis, allergic contact dermatitis.
Treatment regimen
In mild cases, children and pregnant women are advised individual local therapy.Local anti-inflammatory drugs (metronidazole, erythromycin) are used with non-greasy bases (gel, lotion, cream), avoid ointments. Compresses soaked in Lugol's solution and applied for 15 minutes a day until the rash improves.
Read also:Bags under the eyes: causes, symptoms and treatment in women after 50 years
Calcineurin inhibitors may be prescribed (protopic), which are more effective for corticosteroid-induced perioral dermatitis. In some cases, topical antacal drugs have been used, such as adapalen and azelaic acid.
Oral preparations are recommended for more severe forms of perioral dermatitis. Oral antibiotics such as doxyclin and minocycline, with reception 6 to 12 weeks. In refractory and granulomatous forms, may be seen oral isotretinoin.
It was reported that photodynamic therapy effective for perioral dermatitis, although extensive research has not been conducted. Some supplements that reduce skin inflammation, such as vitamin D3 and pycnogenol, can be effective in treatment.
It is important to explain to the patient about the possible risk factors and the development of the disease. These measures help the patient to adapt to the disfigurement of the condition and minimize the risk of relapse. Patients should be advised of the initial worsening of the rash, especially if a corticosteroid has been used previously. Any topical preparations, including cosmetics, should be avoided. Remission can only occur after a few weeks, despite proper treatment.
Forecast
PD is not a life-threatening disease. However, an unexpectedly long treatment period may be required to achieve a cosmetically satisfactory skin condition.
Lilia Khabibulina/ article author
Higher education (Cardiology). Cardiologist, therapist, functional diagnostics doctor. I am well versed in the diagnosis and treatment of diseases of the respiratory system, gastrointestinal tract and cardiovascular system. She graduated from the academy (full-time), she has a wide experience of work.
Specialty: Cardiologist, Therapist, Physician of functional diagnostics.
More about the Author.