Alveolar Proteinosis of the Lung
 Alveolar lung proteinosis is a rare disease characterized by the accumulation of protein-lipoid substances in bronchioles and alveoli. This disease usually affects men from 30 to 35 years. Less commonly, the disease occurs in women, children, and in the elderly.
Alveolar lung proteinosis is a rare disease characterized by the accumulation of protein-lipoid substances in bronchioles and alveoli. This disease usually affects men from 30 to 35 years. Less commonly, the disease occurs in women, children, and in the elderly.
Causes of the disease
There are a couple of versions regarding the appearance of alveolar pulmonary proteinosis:
- Exocrine function of alveolocytes is broken along with hyperproduction of lipid protein secretion.
- Decrease in the functional activity of macrophages, which leads to insufficient secretion.
- Hyperproduction of surfactant.
- Gynecological pathologies.
- Ecology.
- Bad habits.
Pathogenesis of
The pathogenesis of alveolar pulmonary disease is unfortunately not fully understood. It is assumed that the nature of the disease is viral. The influence of other microorganisms does not have sufficient evidence.
There are a number of versions about the pathogenesis of the disease:
- penetration of plasma normal proteins through the alveolar-capillary membrane. This leads to desquamation of the epithelium;
- initial changes in the alveolar epithelium with fatty dystrophy, necrosis, desquamation;
- increase in local production of immunoglobulins.
In our time it became known that the secret located in the alveoli, with this disease contains free fatty acids and phospholipids. In its composition, it is similar to a surfactant, but it has surface-active properties. That is why it is suggested that the reason for the alveolar pulmonary proteinosis is a decrease in the function of alveolar macrophages for alveolar cleansing and, possibly, insufficiency of bronchial secretion. And the main role was given to the activity of phospholipases.
Pathomorphology of pulmonary alveolar proteinosis
Alveoli of the lungs are filled with granular eosinophilic substances. This substance is rich in lipids, has a sharply positive Schick reaction. In these substances, alveolar macrophages accumulated, which have lipid granules in the cytoplasm. There is no inflammatory reaction in the interalveolar septa. In some cases, patients may be observed around small vessels lymphocytic infiltration.
Clinic of the disease
The disease usually begins with cough and sputum. Cough is characterized by progressive dyspnoea. This in some cases is the only symptom. Patients complain of very high fever, and chest pain. Often there is an increase in the liver, splenomegaly is noted. Patients lose weight.
Separate 2 forms of the disease: acute and chronic.
Symptoms of the first, acute form of the disease: very high temperature, severe sweating, cough. In some cases hemoptysis is observed, then progressive dyspnoea and relapses are observed.
Characteristic signs of the chronic form of the disease are a slow onset, general symptoms such as malaise, weakness, decreased performance, weight loss. Also, patients have a subfebrile temperature, and dyspnea gradually develops. Very often the disease looks like an infectious process in the lungs.
There are not enough physical data for this disease. This is hard or weak, sometimes crepitus. In the late stages of the disease there are: a symptom of "drum sticks", cyanosis.
Passage of the disease is usually chronic, with remissions. In later stages, the development of pulmonary and cardiac deficiencies is possible.
The prognosis of the disease is serious. Sometimes spontaneous cure can occur. The disease in childhood is fatal.
Usually the patient addresses to doctors with such basic reasons: slow, but constantly progressing dyspnea, possibly accompanied by a cough. Cough with a small amount of phlegm, yellowish color. Sometimes cough is accompanied by hemoptysis. Also, the patient complains of subfebrile body temperature, sweating, chest pain, cyanosis, rapid fatigue, weight loss.
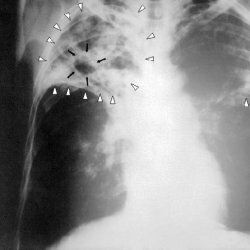
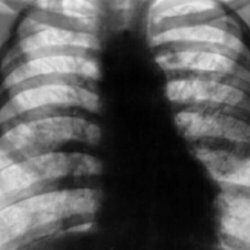
During objective examination, it is possible to determine the shortening of the percussion tone, usually in the lower parts of the lungs. During auscultation, weakened vesicular breathing is observed, rarely - crepitating rales. Clinical and biochemical analyzes do not have any characteristic signs for the disease of alveolar proteinosis of the lungs. In some cases, the blood levels of patients are determined by an increase in the level of calcium and cholesterol. X-ray studies of the lungs show shallow focal shadows that merge. Localization in them is radical. These changes are usually bilateral. Bronchoscopy for this disease is of little informative. The diffusion capacity of the lungs decreases, the restrictive ventilation disorders begin to progress slowly, while hypoxemia is observed during physical exertion.
Diagnosis of alveolar lung proteinase
An accurate diagnosis of the disease can be made only after a lung biopsy.
To make a diagnosis, it is necessary to take into account clinical, laboratory and radiological studies.
Radiographs with pulmonary alveolar proteinosis usually show fuzzy focal shadows in the lower or middle pulmonary fields on both sides. In some cases, they are similar to shadows, as with acute swelling of the lungs. Very rarely, with this disease, one-sided darkening occurs. Patients can find cysts and atelectasis.
Functional state of the lungs during the disease by pulmonary alveolar proteinosis is often not violated, their diffusion ability can vary.
Peripheral hemogram in adult patients with pulmonary alveolar proteinosis does not change; in children, lymphopenia is observed;Increased ESR.In the blood serum of patients with pulmonary alveolar proteinosis, the level of lactate dehydrogenase is increased, and sometimes the content of immunoglobulins is lowered.
Treatment of Alveolar Proteinosis of the Lung
Corticosteroids and immunosuppressants in this disease are not effective. Since 1964, the lavage of the lungs has been used. For this, the patient is intubated. Do general anesthesia. Then one lung is ventilated with pure oxygen, and another lung is washed with saline solution, which contains enzymes and heparin. The entire volume of liquid will depend directly on the washed area, and will range from 1 to 20 liters. Usually, after effective lavage, positive functional, clinical, and x-ray dynamics are predicted. Depending on the speed and severity of the disease progression, lavage of the lungs should be repeated after 6-24 months.
Prognosis of the disease
During the progression of the disease or in acute forms of the disease in 80% of patients the disease ends with a fatal outcome for a period of 5 years. Favorable prognosis for chronic forms of the disease, timely diagnosis, proper treatment and employment. When joining fungal, viral or bacterial infections, the prognosis of the disease is significantly worsened.