Myocardial infarction - causes, symptoms, treatment
Earlier, statistical data indicated the fact that myocardial infarction in men is more frequent after 60 years. However, in recent years, cardiologists are concerned that this pathology is significantly "younger" and the development of necrosis of the myocardium can also occur in young people 20-30 years of age. Disappointing statistics and the number of deaths from this severe illness - over the past 20 years, they have increased by more than 60%.
On average and young age, men have a greater number of factors predisposing to the development of myocardial infarction. This is explained by the fact that many members of the stronger sex suffer from obesity, lead a sedentary lifestyle, smoke and, unlike women, are more prone to rivalry, clarification of relations with superiors and stresses. Such an unhealthy lifestyle leads to the development of such heart and vascular diseases as hypertension, atherosclerosis, ischemic heart disease and arrhythmia.
According to statistics, only half of patients with myocardial infarction survive to hospitalization, and a third of hospitalized patients die before the discharge due to serious complications. And these disappointing indicators of the level of deaths are almost the same for countries with different levels of emergency and medical care.
Contents
- 1 What is myocardial infarction?
- 2 Causes and risk factors for the development of
- 3 How does myocardial infarction develop? Symptoms
- 4
- 4.1 typical form
- 4.2 Atypical forms
- 5 Treatment
- 5.1 pre-medical first aid in case of myocardial infarction
- 5.2 Providing medical care
- 5.3 therapy of myocardial infarction in a hospital
- 6 Consequences and predictions
What is myocardial infarction?
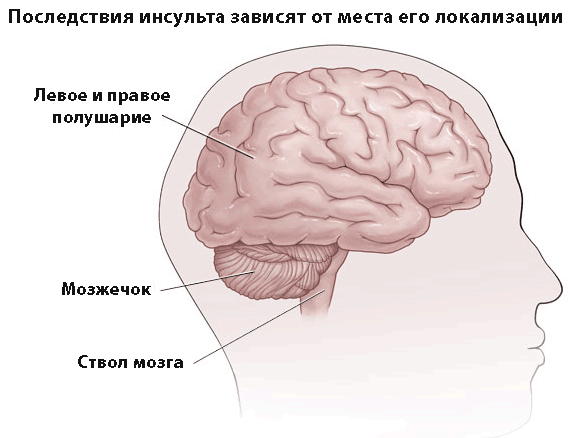
Myocardial infarction is one of the most severe clinical forms of coronary artery disease( ischemic heart disease), which is accompanied by the death( necrosis) of the myocardial part resulting from the cessation of blood delivery to one of the areas of the heart muscle. A similar violation of the coronary circulation, lasting for 15 or more minutes, comes because of complete or relative blockage of one of the branches of the coronary vessels by an atherosclerotic plaque or thrombus. As a result, myocardial cells die, and this affected area of the heart muscle is called myocardial infarction( see Figure 1).

Fig.1 - Myocardial infarction is the affected area of the heart muscle.
Subsequently, the death of the myocardium leads to oxygen starvation of the heart muscle and disruption of the normal functioning of the cardiovascular system as a whole. The patient experiences severe pain in the sternum or heart, which is not eliminated even by taking nitroglycerin, and in the absence of timely medical care, this condition can lead to the death of the patient.
Causes and risk factors for the development of
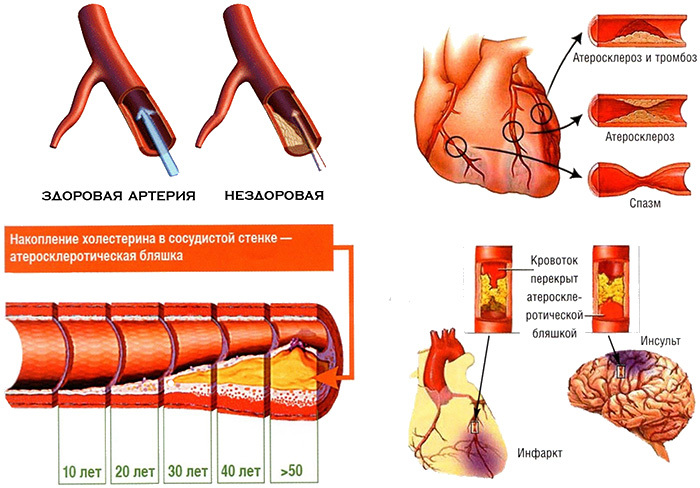
The underlying cause of myocardial infarction is a significant disturbance of blood flow in the arterial vessels of the heart, which leads to ischemia( insufficient blood flow) of one of the sites of the heart muscle and provokes the death of myocardial cells. Such a violation of coronary blood flow can develop due to the following diseases and conditions:
- Atherosclerosis of coronary and coronary vessels. It is the clogging of these vessels with atherosclerotic plaques that is the most common cause of coronary artery disease and the development of myocardial infarction.
- Spasmodic coronary vessels when smoking, taking drugs and unclear reasons.
- Coronary artery thrombosis or fat embolism.
- Surgical obturation of coronary arteries with angioplasty( dissection and ligation of arteries).
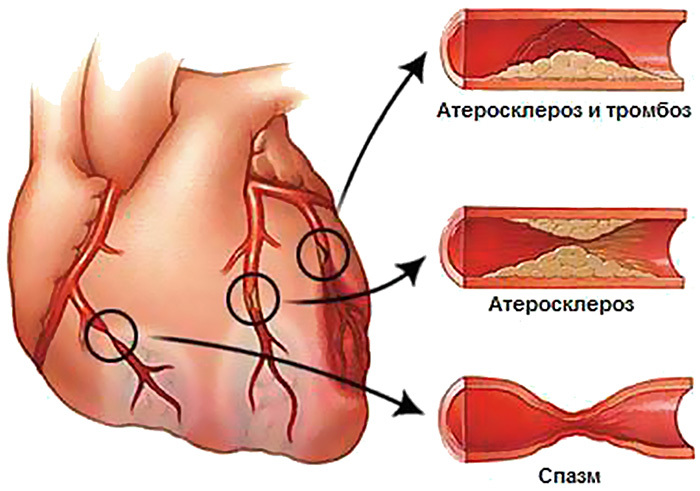
Fig.2 - Conditions preceding myocardial infarction.
An important role in the development of this serious illness is played by such risk factors as:
- overweight;
- smoking;
- alcoholism;
- elevated levels of triglycerides and "bad" cholesterol( LDL) in the blood;
- low level of "good" cholesterol( HDL) in the blood;
- inactivity;
- arterial hypertension more than 140/90 mm Hg. P.
- hereditary predisposition( ischemic heart disease, strokes and heart attacks even in one of close relatives: parents, grandfathers, grandmothers, brothers or sisters);
- bleeding disorders;
- previous myocardial infarction;
- stressful situations;
- cardiac trauma;
- neoplasm( tumors and metastases);
- age over 45-50 years;
- previously transferred streptococcal and staphylococcal infectious diseases;
- excessive physical activity;
- rheumatic heart disease.
The presence of even one of the above risk factors significantly increases the likelihood of myocardial infarction, and a combination of several predisposing factors increases the likelihood of developing this dangerous disease at times.
How does myocardial infarction develop?
Myocardial infarction can begin at the most unexpected moment. Violation of the integrity of the atherosclerotic plaque can be provoked by rapid heartbeat, arterial hypertension, psychoemotional overstrain and physical exertion. The appearance of a crack on an atherosclerotic plaque leads to the deposition of activated platelets and erythrocytes on it. These processes trigger the process of blood clotting and formation of a thrombus. It can grow rapidly and the lumen of the artery begins to narrow sharply. Usually from the moment of formation of a thrombus to complete obturation( blockage) of the coronary artery takes about 2-6 days. These processes are accompanied by the appearance of signs of the pre-infarction state of ( unstable angina):
- spontaneously arising pain attacks in the heart area lasting more than 15 minutes and appearing both on the background of physical exertion and at rest;
- appearance of rapid heart rate, asthma and perspiration;
- increase in the number of attacks of coronary pain throughout the day;
- reduced effect when taking nitroglycerin or the need to take an additional dose to eliminate pain;
- arising on a background of bouts of pain or for 2-3 days unstable signs of myocardial ischemia on the ECG: T wave inversion, depression and ST-segment short-term elevation.
Initially, the necrosis zone captures the top layer of the myocardium. Then it begins to spread to the deeper layers of the heart muscle, heading toward the outer shell of the heart - the epicardium. During the first hour of ischemia in a number of cardiomyocytes, the changes become irreversible. In the next 4 hours, the infarction zone spreads to 60% of the thickness of the affected area of the heart muscle, and over the next 20 hours, the lesion covers the remaining 40% of the myocardium. In some cases, halting the spread of the infarction zone by restoring blood flow in the affected area of the heart by urgent surgical intervention is possible only within the first 6-12 hours.
With the timely start of treatment, the necrosis zone does not increase and by 7-10 days a young granulation tissue appears on the affected area of the myocardium, which gradually begins to be replaced by a connective tissue. As a result, after 2-4 months, a scar appears on the myocardium, which does not resolve and persists throughout life.
Depending on the scale of the affected area, the heart muscle is distinguished:
- large-heart infarcts - the area of necrosis of the heart muscle extends to the entire thickness of the myocardium;
- small-focal infarcts - the area of necrosis of the heart muscle affects not the entire thickness of the myocardium.
Symptoms of
With myocardial infarction, the severity of symptoms depends on the severity and stage of the pathological process. During the course of the disease, the following periods are indicated:
- preinfarction( several days or weeks) - not observed in all patients;
- acute( from 20 minutes to 3-4 hours) - accompanied by ischemia and the formation of the necrosis zone;
- acute period( from 2 to 14 days) - is accompanied by melting of myocardial tissue under the influence of enzymes;
- subacute( from 4 to 8 weeks) - accompanied by the formation of scar tissue in the infarction zone;
- postinfarction - accompanied by the formation of postinfarction scar and the adaptation of the myocardium to the emerging structural changes.
Symptoms of myocardial infarction can occur in a typical and atypical form.
Typical form of
In most cases, in men, myocardial infarction is accompanied by the development of typical clinical symptoms, its signs can not go unnoticed, since the main symptom of the sharpest period is intense compressive pain behind the sternum or in the heart area. Many patients describe it as "burning", "dagger", "tearing".It appears suddenly immediately after a psychoemotional or physical exertion or makes itself felt against the background of absolute rest( for example, during sleep).In some cases, the pain may radiate into the left( sometimes right) arm, neck, lower jaw, or into the area between the scapulae. And its distinctive feature from the pain with an attack of angina is its duration to half an hour or more.
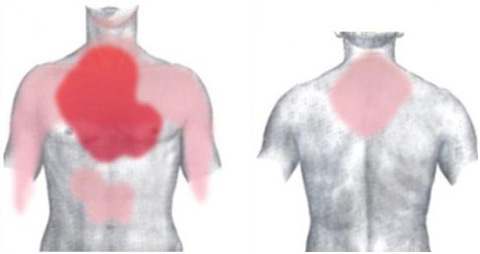
Fig.3 - Localization of pain in myocardial infarction( intensity of color indicates the most common areas of pain).
The patient has complaints about:
- severe weakness;
- anxiety;
- feelings of fear of death.
In some cases, the patient may experience a pre-fainting condition or fainting.
Anginosis in an attack of myocardial infarction is not stopped even by repeated intake of nitroglycerin and other medicines customary for the patient. That is why most cardiologists always advise their patients with the appearance of heart pain lasting more than 15 minutes and are not amenable to elimination of medications customary for the patient, immediately call an ambulance team.
In addition to anginal pain in the acute period of myocardial infarction, the patient has the following symptoms:
- sharp pallor;
- frequent and intermittent breathing;
- frequency of arrhythmia and arrhythmia;
- weak heartbeat;
- plentiful cold sweat;
- appearance of a blue hue on the lips, mucous and skin integuments;
- nausea( sometimes vomiting);
- AD first increases, and then drastically decreases.
Some patients may experience fever of up to 38 ° C or higher during the acute period.
With the onset of an acute period, the pain in most patients disappears. Painful sensations are present only in those patients in whom the development of a necrosis site provoked inflammation of the pericardium or a marked violation of coronary blood flow in the adjacent areas of myocardium infarction.
Because of the formation of a necrosis site in patients in an acute period, the following symptoms are observed:
- fever( over 3-10 and, sometimes, more than days);
- signs of heart failure increase: bluish nasolabial triangle or nails, shortness of breath, darkening in the eyes, rapid pulse, dizziness;
- blood pressure values remain elevated;
- leukocytosis( up to 10-15 thousand);
- increased ESR.
In the subacute period, pain in the region of the heart completely ceases and the patient's condition gradually begins to stabilize:
- passes fever;
- normalization of blood pressure and pulse;
- severity of heart failure symptoms decreases.
In the postinfarction period, all symptoms disappear completely, and there is an improvement in the indices of laboratory tests.
Atypical forms
In 20-25% of patients, the acute period of infarction can occur in atypical forms. In such cases, timely recognition of signs of this life-threatening condition can be complicated, and some patients endure this infarction period on their feet and do not seek medical help. The acute period of the disease in such patients is accompanied by a typical clinical picture.
Cardiologists among atypical forms of acute period distinguish such variants of development of symptoms:
- Atypical pain - the pain is felt in the shoulder or little finger of the left hand, in the neck, cervico-thoracic spine, lower jaw, or in the scapula.
- Arrhythmic - there is arrhythmia and atrioventricular blockades.
- Abdominal pain is felt in the upper area of the anterior abdominal wall and can resemble pain in gastric ulcers or gastritis in nature, and instrumental and laboratory examination methods are needed to establish the correct diagnosis.
- Collapsoid - pain is completely absent, blood pressure drops sharply, dizziness, profuse cold sweat and fainting, the patient can develop cardiogenic shock.
- Cerebral - the patient has paresis of hands and feet, there is a confusion of consciousness, dizziness, nausea and vomiting, speech disorders, fainting or fainting.
- Asthmatic - painful feelings are slightly expressed, the pulse is arrhythmic and weak, the patient has a cough( sometimes, with the separation of foamy sputum) and increasing dyspnea. In severe cases, suffocation and pulmonary edema may develop.
- Ointment - the patient develops pronounced dyspnea, weakness and rapid build-up of edema( up to the development of ascites).
- Bezboleva - the patient feels only uncomfortable sensations in the chest area, he has a pronounced weakness and profuse sweat.
Sometimes, a patient with an acute period of myocardial infarction has symptoms of several atypical forms. In such cases, the patient's condition is significantly aggravated, and the risk of complications increases.
Treatment of
First-aid first aid for myocardial infarction
At the first signs of the development of an infarction, it is necessary to call an ambulance team. The patient should be reassured, give him one of the sedatives: tincture of motherwort, valocordin or valerian, and lay in a horizontal position, lifting his head.
Breathable clothing( belt, tie, etc.) should be removed and sufficient fresh air supplied. To reduce the burden on the heart of the patient, it is necessary to give a tablet of nitroglycerin or another nitro-containing drug( nitrosopere, nitromax, isoket) and a crushed tablet of acetylsalicylic acid under the tongue. Before the arrival of a doctor, the intake of a nitro-containing drug can be repeated under the control of blood pressure indicators. At the rate of 130 mm Hg. Art.and higher the drug intake can be repeated every 5 minutes and before the doctor visits the patient, you can give 3 tablets of nitroglycerin( or 3 doses of a nitro-containing spray).When a pulsating headache occurs, the dose of a nitro-containing drug should be reduced to half, and with a decrease in blood pressure, nitroglycerin is not needed again.
Before the brigade arrives, a non-narcotic analgesic agent( pentalgin, baralgin, spasmalgon or analgin) can be given to the patient before the brigade arrives, and if the patient does not have a history of bronchial asthma and the pulse rate does not exceed 70 beats / minute, one of the drugs of β-adrenoblockers(Atron, atenolol, betacor).
During an attack of a heart attack a patient may become faint, stopping breathing or heart. In such cases it is necessary to urgently carry out resuscitation measures - indirect cardiac massage and artificial respiration( in the mouth or nose).Before they are carried out, the patient's mouth must be freed from sputum or dentures( if any).Perform pressing movements on the lower third of the sternum to a depth of 3-4 cm, continuously with a frequency of 75-80 strokes per minute, and inhale air in the mouth or nose with a frequency of 2 breaths after every 15 clicks.
Provision of medical care to
After the arrival of an ambulance physician, narcotic and non-narcotic analgesics( morphine, trimepiridine, omnopon, dipidolor, fortral) are administered to the patient in combination with atropine and desensitizing drug( suprastin, dimedrol, pipolfen).To ensure the state of rest, the patient is given a tranquilizer( seduxen, Relanium).
To assess the condition, an ECG is performed and if the patient can not be transported to a hospital in the next 30 minutes, thrombolytic drugs( purolase, alteplase, tenecteplase) are administered. After this, the patient is carefully transferred to a stretcher on a stretcher and, before coming to the intensive care unit, he is administered a mixture of solutions of fentanyl and droperidol or talomonal. Throughout the entire transportation, the patient is oxygenated with moistened oxygen.
Therapy of myocardial infarction in a hospital
Medical therapy
After delivery to the department with a prolonged attack of pain, the patient is shown performing an inhalation anesthesia with a gas mixture of oxygen and nitrous oxide. The patient is then oxygenized and administered with such drugs:
- nitro-containing agents( nitroglycerin, isoket, isosorbide, etc.) - are administered intravenously to reduce the load on the myocardium;
- antiplatelet agents( aspirin, clopidogrel) and anticoagulants( heparin, dicumarol, warfarin) - for the prevention of thrombosis, which can trigger the development of a new heart attack;
- β-adrenoblockers( obzidan, atenolol, acebutol, anaprilin, propranolol, etc.) - to eliminate tachycardia and reduce the load on the myocardium;
- antiarrhythmic drugs( rhythmylene, difenine, lidocaine, amiodarone, etc.) - are used in the development of arrhythmia to stabilize the heart;
- inhibitors of ACE( enalapril, lisinopril, ramipril, captopril, etc.) - are used to lower blood pressure;
- hypnotics and sedatives( lorazepam, triazolam, diazepam, temazepam, etc.) - are used when it is necessary to eliminate anxiety and sleep disorders.
If necessary, the treatment plan may be supplemented with other drugs( antiarrhythmic and antihypertensive drugs, adrenoreceptor blockers of the heart muscle, etc.), the selection of which depends on the concomitant diseases of the patient.
Surgical intervention
In case of severe forms of infarction, absence of contraindications and sufficient equipping of the medical institution, the patient can undergo such minimally invasive surgical interventions aimed at restoring blood circulation in the infarction zone as balloon angioplasty, coronary artery or mammarocoronary shunting. They allow patients to avoid the development of serious complications and reduce the risk of death.
With complete blockage of the blood vessel and the impossibility of installing the stent and damaging the heart valves, the patient can undergo an open surgery( with chest opening).In such cases, during the intervention, the valves are replaced with artificial ones and then the stent is inserted.
Conditions for rest and nutrition
In the first day, a patient with a myocardial infarction is shown to observe strict bed rest - the patient is not recommended any motor activity( even body twists in the bed).In the absence of complications, its gradual expansion begins with a third day.
In the first 3-4 weeks after myocardial infarction the patient should observe a low-calorie diet with restriction of animal fats, foods with excessive amounts of fiber and nitrogen compounds, salt and liquid. In the first 7 days after an attack, the food should be served in a grated form, in small portions( 6-7 meals per day).Read more «Nutrition after myocardial infarction».
Consequences and Forecasts of
Most of the deaths in myocardial infarction occur during the first day. With the defeat of 50% of the heart muscle, the heart can no longer function fully and the patient develops a cardiogenic shock and a fatal outcome. In some cases, and with less extensive lesions of the myocardium, the heart can not cope with the arising loads and the patient develops an acute heart failure, which can cause death. Also, an unfavorable prognosis of the outcome of the disease can be observed with a complicated course of myocardial infarction.
The severity of the clinical picture in the first days after a heart attack is determined by the vastness of the zone of myocardial damage, the reactivity of the nervous system and the initial state of the heart muscle. The most dangerous and prognostically severe are the first 3 days of the disease, and it is during this period that the doctor and the medical staff need maximum attention.
In the early days, the patient can develop such severe complications:
- pulmonary edema;
- collapse;
- extrasystole;
- paroxysmal, ciliary or signs of sinus tachycardia;
- ventricular fibrillation;
- pulmonary embolism;
- intracardiac thrombosis;
- thromboembolism of cerebral vessels, kidneys, etc.;
- cardiac tamponade;
- cardiogenic shock;
- thromboendocarditis;
- acute cardiac aneurysm;
- extensive pericarditis.
The following 2 weeks after the infarction is quite dangerous. After the expiration of the acute period, the prognosis for recovery of the patient becomes more favorable.
According to statistics, before hospitalization of the patient, a lethal outcome during the first hour with myocardial infarction is observed in about 30% of cases. Death in a hospital for 28 days occurs in 13-28% of patients, and the fatal outcome within the first year after the infarction occurs in 4-10%( in persons older than 65 years - 35%) cases.
Cardiologist Petrova Yu.
Recommended for viewing: