Inguinal lymphadenitis in men: forms of pathology, causes and treatment
Lymphadenitis is an inflammation of the lymph nodes, most often in the groin, neck and underarm area, caused by the ingestion of a pathogenic microflora or products of its vital activity into the lymph node. There are primary and secondary lymphadenitis, specific and nonspecific.
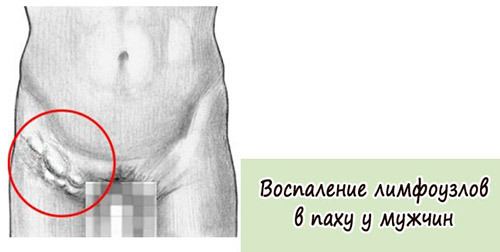
Lymphadenitis - swollen lymph nodes, most commonly caused by the ingress of pathogenic organisms in them
Content
- 1 Causes
- 1.1 nonspecific lymphadenitis
- 1.2 specific lymphadenitis
- 2 disease development
- 3 Symptoms lymphadenitis
- 3.1 nonspecific form
- 3.2 specific form
- 3.3 Chronic
- 4 Diagnosis
- 5 Treatment
- 6 Complications
- 7 Prevention
Causes of
Inguinal lymphadenitis occursFor various reasons: from damage to the lymph node itself to the introduction of pathogenic flora with blood and lymph. Also this disease is a diagnostic sign of some pathologies.
Nonspecific lymphadenitis
Non-specific lymphadenitis can be caused by a different pathological microflora, which, with blood flow, enters the lymph node( secondary lymphadenitis) or directly from the site itself( primary).In this case, staphylococci and streptococci often occur in the development of lymphadenitis, which can enter the lymph node from other parts of the body - purulent wounds, abscesses, phlegmon, trophic ulcers and even untreated caries. If we talk about inguinal lymphadenitis, then most often microbes can get into the lymph node through the wounds on the feet and on the genitals.
Specific lymphadenitis
This form of pathology has a different nature - it is based on the development of inflammation specific microorganisms that cause a certain disease, a complication of which becomes lymphadenitis. In this case, the inflamed lymph node can become a diagnostic sign - with tuberculosis, syphilis, actinomycosis or gonorrhea, as well as chlamydial infection. In this case, treatment should be directed to the source, and inflammation of the lymph node can go away by itself.
Development of the disease
Lymphadenitis of any origin can have acute and chronic course. The acute course is characteristic of the nonspecific form of the disease. In the acute current, there are usually three stages:
- Catarrhal. The lymph node increases in size, the skin turns red, the shells of the sinuses( formation inside the lymph node) are damaged.
- Hyperplastic. At this stage, the node is impregnated with serous contents, leukocytes are attached to it - in case of unfavorable course, pus will form. At this stage, the inflammatory process is limited to the capsule of the lymph node.
- Purulent. At this stage, the lymph node is filled with purulent contents, which after some time breaks into the surrounding cellulose. This threatens the development of a diffuse purulent process, which can be cured only through surgical intervention. Given the location of the inguinal lymph nodes and the proximity of various organs, the purulent stage can cause great problems, so it is necessary to eliminate the inflammation before going into this stage.
Symptoms of lymphadenitis
Nonspecific form of
Symptoms of acute nonspecific lymphadenitis are similar to those of other purulent inflammations - abscesses, phlegmon. They usually appear during the purulent stage of inflammation:
-

With acute lymphadentitis, all the symptoms of an organism's intoxication manifest themselves( temperature, chills, etc.)
high fever;
- headache;
- loss of appetite;
- general malaise;
- increase of the affected lymph nodes, blurring of their contours;
- pain when moving in affected nodes.
Acute inguinal lymphadenitis is characterized by severe pain in all movements, erections. Sexual life during the period of the disease is impossible because of the severe pain syndrome.
Specific form of
With a specific form of inflammation, there are some differences:
- in gonorrhea nodes sharply enlarged and very painful;
- with tuberculosis is most often observed purulent and necrotic degeneration of lymphatic tissue;
- with syphilis nodes enlarged and aching, but not inflamed;
- in the infection of chlamydia in the inflammatory process involves several lymph nodes;
This is why inflamed nodes can serve as a diagnostic sign when diagnosing.
Chronic form
Chronic form of lymphadenitis differs less aggressive course. In chronic form, the lymph node is slightly swollen, almost painless to the touch. Symptoms of malaise are absent or mild. But do not forget that the chronic form can move into acute, so any form of the disease should be subjected to research.
Diagnosis
The diagnosis of lymphadenitis is usually based on a typical clinical picture and anamnesis. Diagnosis of purulent inflammation with the spread of pus in the subcutaneous fat reduces to finding the primary focus. When the shape is diffuse during palpation, one can hear crunches - one of the signs of purulent fusion of the node.
If the disease is slow, a tissue biopsy may be required to determine the pathogen.
In a specific form, the diagnosis is made based on certain laboratory tests. For example, gonorrhea will look for gonococci, with tuberculosis - Koch's wand, with syphilis - pale treponem. In this case, the nature of the diagnosis is determined by the primary disease.
Treatment of
The method and success of treatment directly depend on the stage of the disease. The slight inflammation that still "sits" in the capsule can easily be cured by a conservative method. Purulent inflammation is treated only by surgical intervention:
-

Antibiotics
are used in medicinal therapy of lymphadenitis. Conservative treatment. It is shown in the catarrhal and hyperplastic stage of acute nonspecific lymphadenitis. Includes applying cold compresses to the inguinal lymph nodes, antibiotic therapy, taking NSAIDs and analgesics, as well as UHF therapy and a balanced diet( rich in vitamins).Treatment of a specific form involves the treatment of a primary focus( antibiotics against gonorrhea, syphilis, chlamydia).
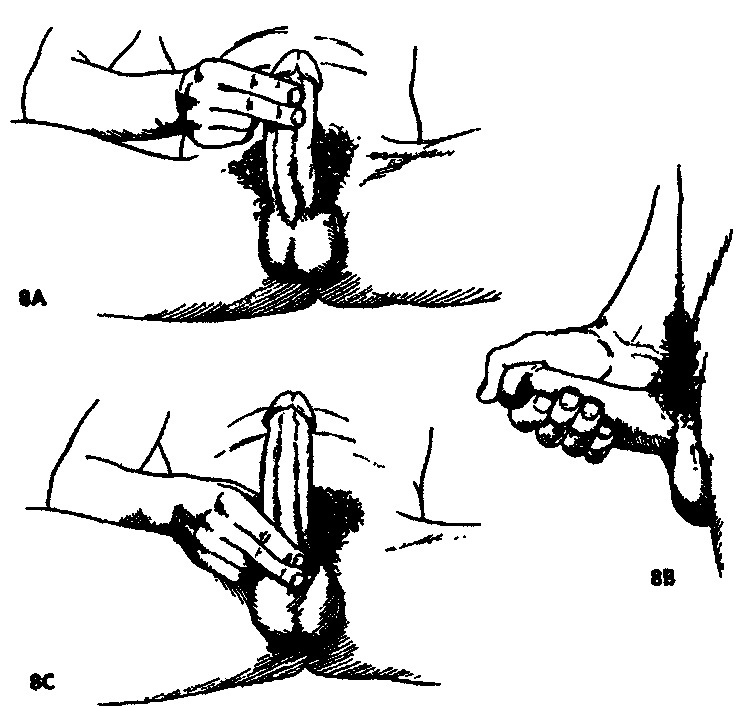
- Operative intervention. Surgery is indicated in the purulent stage of lymphadenitis. Includes an autopsy purulent focus, cleaning the cavity from the products of decay, setting drains for wound washing, adequate antibiotic therapy, measures to remove toxins from the body, as well as bed rest. The complexity of the operation depends on the location of the lymph node. Inguinal lymph nodes are located in the region with a rich network of blood vessels and nerves, so their removal( especially after the spread of pus in the subcutaneous fat) is somewhat difficult. Therefore, it is advisable to begin treatment as early as possible.
Complications of
Inguinal lymphadenitis can give many complications if you do not ask for help in time:
- inflammation of the lymphatic vessels - linghangitis, which adversely affects the condition of the lymph flow in the inguinal region;
- breakthrough pus in the surrounding space, the formation of a spilled focus - adenoflegmon;
- impregnation of the node with blood;
- decomposition with inflammation of nearby tissues;
- necrosis of surrounding tissues;
- involvement in the purulent process of neighboring nodes;
- sepsis as a result of contact of pathogenic microflora with blood;
- thrombophlebitis - inflammation and thrombosis of veins;
- formation of lymphatic fistulas.
Prevention
There is no specific prevention of inguinal lymphadenitis. It is necessary to observe the general rules:
- in time to handle cuts and abrasions on the feet and feet;
- in time to seek the help of a surgeon in the presence of purulent lesions on the legs or in the groin area;
- use condoms during sex( prevention of gonorrhea, chlamydia, syphilis).
Recommended for viewing: