Pericoronaritis
 Pericoronaritis ( in some sources - pericoronitis) is an inflammatory process that takes place in the gingival hood and soft tissues around the erupting wisdom tooth, mainly on the lower jaw. Complicated by purulent process( purulent pericoronaritis), the spread of infection in the surrounding space, purulent dissolution of bone tissue.
Pericoronaritis ( in some sources - pericoronitis) is an inflammatory process that takes place in the gingival hood and soft tissues around the erupting wisdom tooth, mainly on the lower jaw. Complicated by purulent process( purulent pericoronaritis), the spread of infection in the surrounding space, purulent dissolution of bone tissue.
Reasons for pericoronaritis
Pericoronaritis occurs most often with teething wisdom, especially on the lower jaw. Problems with them arise in 4 out of 5 cases. Since wisdom teeth erupt in the last place, they give people the most discomfort, because they are placed differently in the jaw( vertically, obliquely or horizontally), often grow incompletely( it may seem a third or half the size of the crown of the tooth) and damage the surrounding softTissues and adjacent teeth.
Why is teething wisdom so problematic? This is explained by the physiology of our body: in modern man the jaw is much smaller than that of ancestors, and the size of the teeth has remained the same. Therefore, wisdom teeth do not grow according to the standard timing of eruption. And with delayed eruption, new obstacles are added: a thickened mucous membrane over the tooth, dense walls of the gingival hood, and also lower growth factors of the organism as a whole.
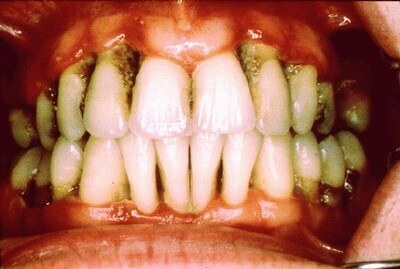
But why does pericoronaritis occur? Pericoronaritis always appears with the accumulation of plaque in the space between the wisdom tooth and the gum covering it - the gingival hood. Dental plaque, including the remains of food and accumulation of bacteria, can not be fully extracted completely. Chronic trauma of this part of the mucous membrane during chewing promotes the appearance of inflammation of soft tissues. Inflammation leads to swelling and soreness of the mucous membrane.
Symptoms of pericoronaritis
To ensure that pericoronaritis does not become a surprise, you must regularly visit a dentist. He will be able to assess the state of wisdom teeth and gingiva hoods over them. If necessary, the doctor will prescribe an X-ray examination, which will determine the direction of growth of the wisdom teeth and the possibility of inflammation of the gingival hood.
Symptoms of pericoronaritis depend on the stage of development of inflammation. With the initial pericoronaritis, it is not easy to detect symptoms, but it is possible. These symptoms are as follows:
- Swelling of the gums. Most often this sign appears one of the first. Around the wisdom tooth and above it the gum increases in size. This is felt when closing the mouth, when the teeth are closing, and the last teeth of the upper jaw are pressed against the swollen gum.
- Pain when brushing teeth and touching. When chewing and with active cleaning with a toothbrush, an inflamed gingival hood is bruised, which is accompanied by unpleasant or painful sensations.
- Unpleasant odor from the mouth. Remains of food that fall under the hood of the gingiva, begin to be processed by bacteria. The products of microbial activity give a characteristic putrefactive odor.
If the pain in the region of the erupting wisdom tooth has become permanent, then one can assert about the further development of the process and the transition of pericoronaritis to the next stage. There are also new symptoms:
- There is a chronic noisy pain in the place of the eruption of the tooth. Pain can be given in the ear or temple.
- The mouth can open with difficulty, because the chewing muscle swells.
- When swallowing food, pain also arises due to edema of half of the near-pharyngeal space and a decrease in the lumen of the pharynx.
- Swelling of the soft tissues becomes larger, the swelling of the cheek is noticeable externally.
- Submandibular lymph nodes increase, when touching painful.
- The general condition of the body is weakened, the temperature can rise to 37-38 degrees, there is a headache.
If you saw in the mirror that the last tooth on the lower jaw is partially or completely covered by the gum - swollen, reddened, then you need to go to the dentist to confirm the diagnosis and determine the tactics of treatment, and before taking the doctor to follow the recommendations for the treatment of pericoronitis at home.
As almost all inflammatory dental processes, pericoronaritis has two forms: acute and chronic.
The acute form of pericoronaritis is characterized by primary, rapidly developing symptoms. For 2-3 days the pain or discomfort in the area of the wisdom tooth becomes not whining, but acute. From under the inflamed gingival hood covering the tooth, there is pus with a characteristic unpleasant odor. Touching the gums causes a sharp attack of pain, giving in the ear, temple or upper jaw. Chewing on the side of the erupting tooth becomes difficult, as opening the mouth and swallowing becomes painful. Lymph nodes increase, when touched painful.
In case of incorrect treatment tactics, prolonged treatment at home or absence of treatment, acute pericoronaritis passes into a chronic form. Then the inflammation periodically then subsides, then becomes aggravated. There are practically no complaints in the remission phase. The number of symptoms is getting smaller. There is an enlarged, painful when touching the submaxillary lymph node. The mouth opens freely, painlessly. The gum hood and the gum of wisdom surrounding the tooth are reddened, however, painless or slightly painful. Periodically, a quantity of serous fluid appears from beneath the gingiva hood.
The acute stage is characterized by acute pericoronaritis. From under the hood comes out regularly pyogenic fluid, because of which you can feel the characteristic odor from the mouth. The wisdom tooth and the adjacent tooth become mobile, because of the inflammation under them the bone tissue dissolves. The mucous membrane around the wisdom tooth is reddened, swollen. Due to chronic trauma of the mucous membrane, the outflow of pus from under the gingiva hood can be disturbed. This often causes the spread of purulent inflammation in surrounding tissues and spaces.
Infection, located in the mucosa of the gingival hood, when spreading into adjacent spaces, can cause serious complications:
- abscesses( when the purulent focus is encapsulated) and phlegmon( purulent inflammation becomes diffuse);
- purulent lymphadenitis( the lymphatic vessels enter the lymph nodes, causing their inflammation);
- osteomyelitis of the lower jaw( purulent inflammation and softening of bone tissue);
- actinomycosis( formation of multiple granulomas and fistulas in soft tissues);
- ulcerative stomatitis;
- periodontitis of the wisdom tooth itself and the neighboring, ahead of the second molar.
Treatment of pericoronaritis
If you find symptoms of the initial stage of pericoronaritis, you can try to remove them at home before visiting a dentist using anti-inflammatory products of plant origin and antisptic medicines. All solutions must necessarily be at room temperature, so as not to provoke a burn of the inflamed mucous membrane. It is also possible to perform applications of anti-inflammatory gels and ointments on the gingival hood and the surrounding gum.
It is important not to forget that any treatment at home leads only to the removal of symptoms of pericoronitis. Completely remove the plaque from the gingiva hood, thoroughly clean and rinse the space under it will only be a dentist.
Treatment of pericoronaritis in a dental clinic will depend on the stage of the disease. At the initial stage, the gingival pocket under the hood is washed with weak solutions of antiseptics( Furacillin, Potassium permanganate, Chlorhexidine bigluconate, Miramistin and others), rinses, mouth baths and anti-inflammatory gels and ointments are prescribed.
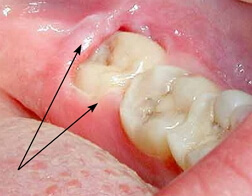
In more severe stages of pericoronaritis, dental intervention is necessary. The dentist performs an examination and appoints an X-ray examination( a sighting intraoral shot, an orthopantomogram or a computer tomogram) to clarify the diagnosis and exclude dental diseases with similar symptoms( chronic pulpitis, chronic periodontitis, neuralgia of the third branch of the trigeminal nerve).On the X-ray image, pericoronaritis is confirmed if inflammatory changes around the root of the wisdom tooth are absent. Also, X-ray diagnosis is needed to determine the direction of tooth eruption.
If the wisdom tooth erupts upwards, has an antagonist on the upper jaw and can participate in a full-fledged chewing act, then the dentist performs an excision of the gingival hood. This manipulation involves anesthetizing and cutting off a portion of the mucous membrane covering the tooth. Excision is performed with a scalpel, a laser device or an electrocoagulator. When excising with a scalpel, a gauze swab should be kept on the wound for 30-40 minutes to stop bleeding. It is preferable to perform laser excision or an electrocoagulator to produce a sealed blood vessel. Excision by such methods is minimally traumatic, and the patient does not experience discomfort after the procedure. As a result, the chewing surface opens, and the plaque and microorganisms cease to accumulate under the hood. After this, recommendations are made for the removal of inflammatory phenomena in surrounding soft tissues - rinses, mouth baths and applications of anti-inflammatory ointments.
If the wisdom tooth erupts not upward, but inclined( resting on the adjacent tooth, in the buccal, lingual side) or "lies" in the jaw bone, which is confirmed radiologically, does not participate in the act of chewing, does not have enough room for eruption, it showsremoval of a tooth.
There is an opinion that wisdom teeth should be left as a reserve as a support for orthopedic construction. This is a general misconception, since the chewing load that can be borne by wisdom teeth is only 2%.If the wisdom tooth is used as a support for the prosthesis with the loss of the lower chewing teeth, excessive loading will lead to an increase in the mobility of the supporting teeth, their subsequent loss and replacement of the prosthesis. Therefore, leaving the wisdom tooth when testifying to its removal, it should be remembered that this is a risk.
After removal of the symptoms of acute pericoronaritis, the tooth is removed, the well is cleaned and sutured. The operation is performed under local anesthesia or general anesthesia, depending on the complexity of the operation and the patient's wishes. The wisdom tooth can be removed completely( for example, with the corresponding position of the roots) or in parts( with branched roots, horizontal or semi-horizontal position of the tooth in the hole).After extraction of the tooth, a bone-plastic material or platelet plasma is placed in the well for rapid restoration of bone tissue. In such cases, it is often necessary to suture the socket, but, with a simple tooth removal, it is possible to leave it for self-healing. Closure of the hole after removal usually takes two to three weeks. After surgery, it is important to follow the recommendations of a dentist - taking antibiotics, antihistamines, mouth baths and applying anti-inflammatory ointments.
To avoid all problems associated with teething wisdom, you must regularly visit a dentist. The doctor can prematurely detect the inflammation of the gingival hood over the wisdom tooth, perform X-ray diagnostics and choose the right treatment tactics. The removal of the tooth, carried out in time, relieve the discomfort associated with a difficult eruption, and will allow to avoid repeated excision of the constantly formed hood.