Chronic periodontitis
 Chronic periodontitis is a long-lasting inflammation in conditions of infection, overloading periodontal tissues, irrational endodontic treatment, occurring in the tissues near the tooth, manifested by the rupture of the periodontal ligament, destruction of the cortical plate of the alveolus and bone damage. Chronic periodontitis is the final stage of acute periodontitis, or, bypassing this level, is transformed into a chronic direction at once.
Chronic periodontitis is a long-lasting inflammation in conditions of infection, overloading periodontal tissues, irrational endodontic treatment, occurring in the tissues near the tooth, manifested by the rupture of the periodontal ligament, destruction of the cortical plate of the alveolus and bone damage. Chronic periodontitis is the final stage of acute periodontitis, or, bypassing this level, is transformed into a chronic direction at once.
For the development of this pathological process, the microflora must arrive long and regularly in the dental cavity. The source of intake in most teeth with the last stage of caries or its complication( pulpitis).Proceeding for a long time in the tooth as a microorgan, the microflora secretes endo- and exotoxins, triggering the hypoergic-type inflammatory process, causing a sensitization reaction of the organism, manifested by destruction and regeneration processes. This subsequently causes the development of the following forms: chronic fibrous periodontitis, chronic granulating and granulomatous periodontitis.
Diagnostics is performed on the basis of clinical and additional methods of medical examination( X-ray examination, electrodontometry, histological examination, fistulography, gutta-percha probe test).
Treatment of chronic periodontitis includes the stages of cleansing and sealing of the tooth canals, stimulation of regeneration of the affected bone, if necessary, surgical intervention is added.
Causes of chronic periodontitis
Causes of chronic periodontitis distinguish local and general. Local - it's infectious agents( microflora) and non-infectious( trauma occlusion, toxic and allergic resonance of the body to drugs and substances spent in the healing process of the tooth canal).
Chronic infectious periodontitis is born on the background of the poliobacterial flora present in the oral cavity. Dominate the complexes of microorganisms: staphylococci, streptococci, Klebsiella, veynelolla, E. coli, yeast-like fungi, etc. Microbial flora in periodont enters intradental and extradental way. Intradentally, the microflora penetrates into the periodontal tissue through the tooth cement, the dentinal tubules, the cortical plate of the alveoli( through the tooth-gum connection in diseases of the periodontal tissues) or through the tooth canal( in pulpitis).The extrasound pathway is possible bypassing the lymph and blood. The passage of infection from regional regions is also possible. Chronic apical periodontitis is formed against the background of accumulation of these agents in the periodontal zone.
Noninfectious causes of chronic periodontitis are triggered by congestion of periodontal tissues and irrationally performed endodontic treatment. Overloading causes an overstatement of the occlusion when the sealing conditions are not observed, the installation of removable and non-removable devices. Also, in the absence of a multitude of teeth, the pressure transferred during chewing takes the nearest ones. In the environment of a prolonged increase in pressure on the periodontium, inflammation begins to be triggered, chronic fibrous periodontitis is formed. When the infection is added to the apex zone, the organism includes destruction processes( osteoclast cells work) and regeneration( osteoblasts, respectively).There is uneven dissolution and reposition of the bone. The organism tries to distinguish the inflammation by the development of granuloma, chronic granulomatous periodontitis develops. The rapid action of aggressive factors allows the inflammation to break through the obstacle, with uneven distribution across the bone, forming a chronic granulating periodontitis.
Non-rational endodontic treatment as an option of non-infectious causes causes the formation of chronic periodontitis after prolonged action of agents in the apex zone. At the initial stage, a periodontal injury can be caused by endodontic instruments during cleaning and filling of the tooth canals. It is not excluded during the healing process the output of aggressive medicines( resorcin, formalin, arsenic) or material per apex. This contributes to the development of a toxic periodontal response and an allergic response in the future.
To general causes of development include diseases of body systems: diseases of digestive organs, nervous, endocrine, cardiovascular systems, metabolic diseases.
Symptoms of chronic periodontitis
In an environment of long-term systematic effects of causal conditions, mainly traumatic occlusion, the occurrence of chronic fibrous periodontitis, characterized by mild clinical manifestations. The patient occasionally notices aching pain. Percussion does not reflect changes in the tooth. Probably a change in the color of the tooth.
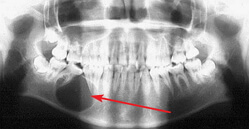
Chronic fibrous periodontitis on the x-ray is indicated by an expansion of the gap and a violation of the clearness of the outline of the upper wall of the alveoli.
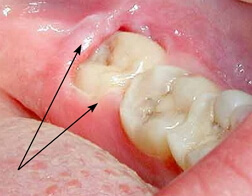
Chronic granular periodontitis is characterized by rapid development. The patient notices occasionally increasing pains, aching directions, exacerbated by the action of hot food, tapping and biting. Percussion with chronic periodontitis gives an approving reaction, it is permissible lability of the tooth. When visualizing the gums, you can see swelling and redness, the presence of a fistula with detachable contents. When taking a histology, exudate is possible serous-bloody or bloody-purulent. Fistula is detected in the oral cavity or in regional soft tissues. Perhaps the closure of the fistula and the chances of escalation in the future. On the roentgenogram, bone deformity of the "flame-like shape" is visualized.
Chronic granulomatous periodontitis occupies an intermediate position among these forms, characterized by the formation of a granuloma filled with granulation tissue, is slow and virtually asymptomatic. It is installed on the x-ray. In the future, the large-scale disappearance of the bone is complicated by a fracture of the jaw. Exacerbation occurs with a decrease in the reactivity of the body and enhance the action of antigens. X-ray data correspond to indications outside the exacerbation. The pain syndrome is intensifying, the swelling of regional tissues, lymphadenitis, and intoxication of the body join.
Forms of chronic periodontitis
Chronic fibrous periodontitis is distinguished by the fact that the periodontal filaments connecting the tooth gradually, under the influence of causal factors, are replaced by coarse fibrous fibrous tissue. Inflammatory process, localized in periodontium, presses on the cortical plate of the alveoli, which then causes dilatation of the periodontal gap. On X-ray, the periodontium is normally visualized as a thin slit between the root of the tooth and the alveolus of the bone. Chronic fibrous periodontitis is visualized in the form of an expansion of this gap.
Chronic granular periodontitis is characterized by the replacement of bone with a granulation tissue, which visually looks like a fleshy, crimson tissue of red color. Granulation tissue grows rapidly, breaking through a compact plate of the alveoli, and granulation with infiltrative growth penetrates into the underlying bone, with subsequent exposure to soft tissues. Fistula is defined in the oral cavity or dermal fistulas can be indicated in the region of the chin, cheekbones, cheeks, inner corner of the eye, neck. Exudate exudates from the mouth or granulation tissue swells. After the fistula is tightened by a scar. On the X-ray, darkening is determined in the apex region of the flame-shaped form. At these places, the bone is missing and replaced with a granulation tissue.
Periodontal abscess or chronic granulomatous periodontitis is similar to a follicle from a capsule filled with pus. Against the background of the long-term pressure of the granuloma containing pus, melting of the latter occurs on the bone, and the granuloma with the tissue growing in it moves to the zone of emptiness. There are processes of bone destruction, growth and progression of the granuloma into the newly formed cavity. There is a growth gradation: in the 0.5 cm boundary - granuloma, 0.5 - 1 - cystogranuloma, beyond the 1 - cyst. The cavities of all formations are filled with pus. Sometimes the size of the basal cyst is significant and can establish a jaw fracture under the effect of minor trauma. Also subdivided granulomas in the correlation from the location: subperiosteal, submucous and subcutaneous. On roentgen it is defined as a darkening of a rounded species, with distinct boundaries in the apex region. The blackout is a cavern filled with pus, smooth edges - a capsule not combined with the bone.
Chronic periodontitis in the acute stage
Long-term chronic apical periodontitis is prone to exacerbation. Escalation is possible with granulating and granulomatous forms. In the clinic, this is manifested by an increase in pain, tearing, pressing character, progressing when touched to the tooth, irradiating into closely located teeth, in the direction of the ear or an opposing jaw. The crown of the tooth shows a noticeable destruction, filled with brittle, highly colored content. When probing is likely to find the mouths of the tooth canals, painless, detritus smell, detritus, or a bulky seal is visualized, the size and position of which presupposes the probability of past endodontic healing. The tooth is variable in color, mobile. There is a swelling of local and regional tissues, lymphadenitis, symptoms of intoxication.
Causes of exacerbation: rupture of the capsule of the periodontal abscess, the failure of the flow of pus from the site of inflammation, the fall of the body's immune system. Chronic granulomatous periodontitis, as noted earlier, is characterized by the presence of a capsule of compact connective tissue filled with pus, excessive pressure on the tooth will automatically transmit tension to the delimited focus of inflammation. From the inside, the formation is done with pus, and biting the tooth causes an increase in the onslaught of pus. Excessive pressure will contribute to the violation of the integrity of the shell and the release of pus into the underlying tissue, which contributes to the aggravation of the process.
Chronic granulomatous and granulomatous periodontitis is characterized by the regular occurrence of pus, which clinically passes preferably asymptomatically, along with the presence of the outlets for pus: through the fistula moves into the oral cavity or local soft tissues, or through channels into the carious cavity. When sealing the fistula or filling channels( food remains), accumulation of pus occurs at the site of inflammation, which increases the bursting of tissues and the formation of pain. With a decrease in the reactivity of the body, reserve forces that retard the increase in microflora during periodontitis of the teeth decrease. Further, the infection spreads, causing escalation.
Diagnosis of chronic periodontitis
Clinical trial data indicating chronic apical periodontitis should be confirmed by objective examination, instrumental methods of investigation. The initial visit to the dentist includes an analysis of the patient's complaints of pressing pain or lack of it, strengthening with biting, changing the color of the tooth, the presence of education on the gum or face. Anamnesis collection allows you to find the cause of chronic periodontitis. The clinic visualizes the causative tooth with a carious cavity or an extensive seal, the probing is painless, the percussion is usually positive, the temperature sample is negative or positive for heat, the palpation of the transitional fold is painful, the mucous membrane is hyperimaged, the fistula is visualized.
Additional examination methods: electrodontometry, fistulography, radiography, histological examination.
Electrodontometry is a survey method based on the detection of the level of sensation of pulp to electric current. With all types of periodontitis, pulp necrosis occurs, and if there is a stimulus of more than 100 μA, there is no reaction to pain. Chronic granulating periodontitis is additionally diagnosed by fistulography.
Fistulography is one of the methods of X-ray diagnostics, in which a contrast composition is produced at the mouth of the fistula in order to find the direction of the moves and connect them with regional tissues. Before the examination, radiovisiography in the facial and profile is performed. Introduce oily( Iodolipol, Lipiodol) or aqueous( Diiodon, Diododrast, Cardiotrast, Urografin, etc.) composition of the contrasting suspension( in correlation from the width of the fistula).The introduction is carried out under X-ray control. A gutta-percha probe is also used to identify the causative tooth through the fistula. The essence of the method - select a gutta-percha pin( the thinnest), injected through the mouth of the fistula slowly to the limit. Perform radiography. On it, and will see a tooth with inflammation.
Chronic apical periodontitis is mainly diagnosed by X-ray examination. In the fibrous form, the periodontal gap broadens as the darkening, fuzziness of the contours of the bone adjacent to the tooth.
Chronic granular periodontitis is clearly diagnosed by dimming the "flame-like shape" in the region of the apex, the gap in the remaining direction is stretched, which also manifests itself as a dimming.
The granulomatous form is verified as a rounded obscuration, with distinct outlines in the apex zone. Exacerbation of chronic forms on the X-ray will show data corresponding to forms outside the exacerbation. Histological examination is performed with the task of identifying chronic periodontitis and actinomycosis. Produce a fence of exudate( smear, imprint).Differential diagnosis is performed with chronic pulpitis, mycosis, face and neck fistulas, and inflammation of the jaws.
Treatment of chronic periodontitis
In the treatment adhere to therapeutic or surgical tactics.
Therapeutic treatment of chronic periodontitis is possible with the patency of the tooth canals. Complex treatment involves the phased elimination of the inflammatory part, the destruction of the microbial flora on all fronts of the inflammation: the leading canal of the tooth, its branching( dentinal tubules), periodontium;And stimulation of regeneration of periapical tissues. Exudate from all places must be withdrawn. At the end of the healing it is necessary to achieve isolation of the space of the tooth canals from the periodontal gap. In the treatment of exacerbation of chronic periodontitis, it is necessary to initially block the acute phase: it is necessary to anesthetize, along with the ongoing cure.
In the first visit to the dentist, the treatment of chronic periodontitis is performed by opening the cavern of the tooth. For this purpose, a qualitative refinement of the carious cavity or removal of the old filling is performed. Regular disinfection of the working field is necessary. Following the cleaning of the tooth canals from the detritus or root filling, careful antiseptic treatment of not only the canal channels but also of the periapical region is carried out( 3-5% Hypochlorite of sodium, 2% chlorhexidine bigluconate).To increase the antiseptic effect on periodontitis, physiotherapy is used: electrophoresis of antiseptics whose molecules in the suspension produce strongly polarized ions( potassium iodide);Phonophoresis - introduction of antiseptic into microchannels under the influence of ultrasonic waves;Laser - under the influence of laser radiation there are two processes of the same name: sterilization of the tooth canal in view of direct bactericidal action of the laser, separation of atomic oxidants( oxygen or chlorine) arising from the decomposition of more complex molecules under the action of radiation. Next, anti-inflammatory substances are injected on turundas, put a short-term seal. Assign also antibiotics of a wide field of influence( Metranidazole, Ciprolet), NSAIDs( Diazolin, Claritin), analgesics( Ketorol).Chronic apical periodontitis continues to be treated after 2-3 days: a temporary seal is removed, the root canals are processed and sanitized, the medicinal paste is filled with a medical paste for a period of 2-3 months( Calcept, Metapex).
Chronic granulating periodontitis, as well as chronic granulomatous periodontitis, characterized by bone destruction in the apex region, need its repositioning. Calcium in the composition of the therapeutic paste activates the work of osteoblasts, thereby the bone is formed again. At the end of the required time, the final radiography is performed, the root canals are processed, the gutta-percha is filled with a permanent seal. In addition to curing chronic periodontitis, physiotherapy is prescribed: electrophoresis, ultraphonophoresis, UHF, UHF therapy, laser therapy, magnetic therapy.
Surgical methods for the treatment of chronic periodontitis are performed if it is impossible to perform a full endodontic treatment. Priority is given to dental preservation: amputation, hemisection, cystotomy, cystectomy, resection of the apex of the root, etc.
Amputation - trimming of the struck radix to the edge of the transfer to the crown of the tooth.
Hemisection is the removal of a patient radix together with a crown.
Cystotomy is the path of incomplete cyst removal. The shell is opened, letting out the pus, doing antiseptic work and sewing up the mucous flap.
Cystectomy - the removal of cysts one-stage.
Resection of the tip of the radix is a surgical variant of seizure of sites of inflammation and infection, including a pathological site in apex, with protection of the tooth function. The operation of the regular is realized on single-root( incisors, fangs), occasionally in multi-rooted teeth.
Before the operation, the tooth channels are closed with a root seal, there is an X-ray. If you have a history of general diseases, then pre-performed tests( blood, urine, electrocardiography, etc.), the patient receives admission from the necessary doctors. After the operation, desensitizing, anti-edema, anesthetics, immunomodulators and vitamins are prescribed. If it is impossible to preserve the tooth during chronic periodontitis, extraction is performed.