Haemophilus influenzae is the causative agent of pneumonia
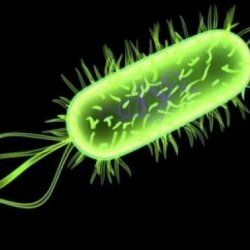 In 1889, during the raging pandemic flu, German bacteriologist Richard Pfeiffer singled out a rod-shaped immovable gram-negative bacterium - a haemophilic influenza rod, and took it for a pathogen of influenza. As a result, the bacterium got its name - Bacillus Pfeiffer. In the 30s, the viral nature of the flu was established and, therefore, it was concluded that the hemophilic rod has nothing to do with influenza, but the name of the "influenza" has been preserved.
In 1889, during the raging pandemic flu, German bacteriologist Richard Pfeiffer singled out a rod-shaped immovable gram-negative bacterium - a haemophilic influenza rod, and took it for a pathogen of influenza. As a result, the bacterium got its name - Bacillus Pfeiffer. In the 30s, the viral nature of the flu was established and, therefore, it was concluded that the hemophilic rod has nothing to do with influenza, but the name of the "influenza" has been preserved.
Later, in 1933, scientists found that the hemophilic rod causes the development of meningitis, pneumonia, arthritis, epiglotitis. At present, about 16 types of hemophilic bacteria and several different serotypes have been identified. Particularly dangerous for humans serotype b. This gram-negative bacterium, capable of forming a protective capsule, so that without being attacked by the human immune system, quietly exists in his body. The presence of a capsule makes the bacterium also almost invulnerable to antibacterial drugs. Hemophilus pneumonia is one of the most serious infectious diseases caused by the so-called "influenza rod", or the hemophilic stick of Pfeiffer.
Sources of infection
The source, or carrier of hemophilia, is a human and only human. The disease is transmitted aerogenically, aerosol, by coughing with phlegm, sneezing and mucus of the nasopharynx. Less often contact-household, for example, through a patient with conjunctivitis. In this case, infection can occur through a handshake, the use of contaminated household items and the like( in children through saliva and infected toys, dishes, etc.) and only from person to person. Penetrating through the nasopharynx, the infection spreads further into the chest cavity, throat or middle ear. Getting into the bloodstream, the infection spreads through the human body, affecting primarily the respiratory system, provokes exacerbation of chronic bronchitis, causes the development of purulent foci in virtually any organs. It is due to the ability of the hemophilic rods to rapidly penetrate into the blood, the course of the disease is especially difficult, often accompanied by various complications, such as pleurisy, bilateral inflammation of the lungs, etc.
Epidemiology
The incidence of hemophilic pneumonia begins, as a rule, with the onset of cold weather, keeps all autumn, winter and captures the cold months of spring. The peak incidence is noted at the end of winter before the beginning of spring.
The main risk groups for the disease are:
- children up to the age of two,( before this age, the immune system of the child does not produce the required amount of antibodies to this kind of infection),
- children on artificial feeding,
- older people aged 60 years,
- People with weak immunity( HIV, oncology, blood diseases)
- people with reduced social status( homeless people, chronic alcoholics, drug addicts)
- people with chronic lung diseases,
- people who underwent surgery for removal fromlezenki.
Exposure to infection with hemophilic infection at an early age is due to the inability of the child's immune system to rapidly produce the required amount of antibodies that are contagious to infection. After recovery in the body of young children, a weak immune response is produced, which does not exclude the recurrence of the disease. In the older age group, the immunity is more pronounced, in adults the resistance to infection is stable and stable.
Symptoms of Hemophilus pneumonia
As a rule, the symptoms of the disease grow gradually, beginning with a slight chill, a slight increase in body temperature, subfebrile fever, nasal congestion with increased discharge. Feeling painful tingling in the side, there is an increasing cough, initially unproductive dry, then intensifying painful with abundant sputum, often rusty. Then there is shortness of breath, pain in the right side of the chest increases, which is worse when coughing, in 50% of cases, pleural effusion joins. The state of health of the patient is rapidly deteriorating. There is a growing weakness, loss of appetite, cyanosis, extremely rare, but there may be vomiting. Sometimes there is a fainting condition.
Diagnosis
When diagnosing hemophilic pneumonia, sputum analysis is performed first. Due to the fact that in order to obtain the most objective results, the analysis should be carried out within the first 2 after receiving the material, and this is not always possible, it is necessary to carry out a number of additional studies. So, it is necessary to conduct an extended blood test with a leukocyte formula and chest X-ray.
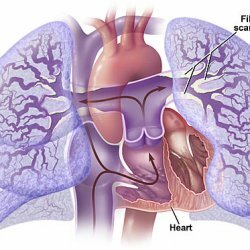
X-ray diagnosis in two projections gives the most reliable results. At a roentgenography the focal infiltration is more often visible in the lower lobes of a lung, characteristic for the given kind of a pneumonia. The pleural effusion is also visualized. A computer tomogram is suitable for insufficient effectiveness of X-ray diagnostics, to confirm the diagnosis.
For laboratory analysis, the secretion of the respiratory tract, sputum, blood culture and pleural effusion, washings from the tracheo-bronchial tree during bronchoscopy is taken. It is established that the results of analyzes and, accordingly, the accuracy of diagnosis are adversely affected by unsystematic and irrational use of antibiotics at an early stage of the disease.
Treatment of hemophilic pneumonia
Treatment is based on established universally accepted protocols and standards with the use of starting antibacterial therapy against possible gram-negative pathogens. The following groups of antibacterial drugs are used: cephalosporins of III-IV generation, III generation aminoglycosides, carbopenems, monobactams, respiratory fluoroquinolines of the latest generation. Rational antibiotic therapy is based on the indication of this causative agent of pneumonia, taking into account its highest sensitivity to the above groups of drugs.