Primary pulmonary hypertension
 Primary pulmonary hypertension( PGH) or Ayrza-Arilago syndrome is a rare disease and occurs in 1-2 cases out of one million. Diagnosis of the disease is difficult due to the fact that the symptoms are similar with more frequent diseases. Etiology is not known, but according to the latest data, PLG refers to hereditary diseases with genetic expectation( BMPR2 gene isolated).That is, with each generation the manifestation of the disease occurs at an earlier age. Women of any age are more likely to develop the disease. There is a family and sporadic form of the disease.
Primary pulmonary hypertension( PGH) or Ayrza-Arilago syndrome is a rare disease and occurs in 1-2 cases out of one million. Diagnosis of the disease is difficult due to the fact that the symptoms are similar with more frequent diseases. Etiology is not known, but according to the latest data, PLG refers to hereditary diseases with genetic expectation( BMPR2 gene isolated).That is, with each generation the manifestation of the disease occurs at an earlier age. Women of any age are more likely to develop the disease. There is a family and sporadic form of the disease.
PLG is characterized by increased pressure in a small circle of circulation, accompanied by changes in precapillary pulmonary arteries and thrombotic lesions. In the absence of chronic heart diseases and chronic thromboembolic pathology, the disease progresses, which leads in a fairly short time( 2-8 years) to right ventricular failure and death.
The disease passes in three stages
- 1 stage. Clinically, almost no manifestation, there is only a slight shortness of breath after physical exertion and is often explained by the lack of training;
- 2nd stage. It is characterized by a decrease in cardiac output. It appears in the form of hypoxemia, dyspnea, syncope appears. Stably high pressure is maintained in the pulmonary artery;
- 3rd stage. It is characterized by right ventricular failure, a drop in cardiac output, venous congestion and peripheral edema.
The variants of manifestation of the disease
- are thrombotic, with the formation of microthromboembolism;
- is plaxogenic with lamination of the muscular membrane of arterioles and aneurysmatic dilatation of arterioles;
- venous-occlusive with venous congestion in the lungs.
Pathological changes
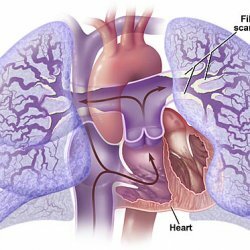
Autopsy can detect pathological changes in the right heart and lung. In large vessels, sclerotic plaques are found. Since small pulmonary arteries are involved in the process, the muscle layer is hypertrophic, fibrosis and intimal hyperplasia are observed. Sometimes necrotizing pulmonary arteritis is found. The number of small arteries and capillaries is reduced, the thickening of the basal membrane of the alveolar capillaries and the hypertrophy of the medial pulmonary arteries are characteristic.
PLG has some similarity with recurrent pulmonary embolism. The difference lies in the fact that thromboembolism reveals recanalized thromboemboles, but there are no plexiform changes. There is also a similarity to veno-occlusive disease of the lungs.
Predisposition
As mentioned above, PLH is a hereditary disease. Also, such pathologies as
- collagen vascular diseases,
- HIV,
- , cirrhosis accompanied by nerve hypertension,
- rheumatoid arthritis,
- unidentified thromboembolism,
- pulmonary embolization are predisposed to its development.
In terms of risk factors, according to the latest data,
- may cause some dietetic agents( appetite depressants) such as fenfluramine, phentermine,
- to use rapeseed toxic oil,
- for taking anorexigens( aminorexa tromat),
- some herbal preparations containing Crotalaria plant,
- oral contraceptive intake.
Symptoms of
Clinical manifestations of PLH, such as hypoventilation, chest pain arising from physical exertion, can be explained by neurotic disorders. Later, shortness of breath, weakness, increased fatigue, there is hoarseness of the voice due to compression of the laryngeal nerve due to an increase in the pulmonary artery, peripheral edema, palpitation.
A physical examination reveals epigastric pulsation due to an enlarged right ventricle of the heart, a galloping atrial rhythm is heard, which is better audited in the lower sections of the sternum to the left. With ascultation, a strengthened pulmonary component, right-sided gallop or triguspidal regurgitation is revealed. Systolic murmur on the pulmonary artery is sometimes observed.
When radiographing the chest, pulmonary artery enlargement, right ventricular and right atrial enlargement, as well as a sharp narrowing of the branches of the pulmonary artery are determined.
Electrocardiographic examination shows right ventricular overload, axis deviation to the right, amplification of S waves in the lower leads, R waves larger in lead V1., Inversion of T wave in right thoracic leads. The best test for the observation of PLG is Doppler echocardiography.
Differentiation of
In order to establish the correct diagnosis of PLG, it is necessary to exclude other known diseases:
- chronic bronchopulmonary diseases with pulmonary heart formation;
- sarcoidosis;
- pneumoconiosis( silicosis) - accompanied by hypoxic pulmonary hypertension;
- congenital heart defects( cardiac catheterization and echocardiography for differentiation);
- pulmonary embolism( detected by angiopulmonography or radioisotope scanning of the lungs);
- pulmonary artery stenosis;
- Eisenmenger syndrome, if it is accompanied by a defect of the interventricular septum, somewhat resembles PLG;
- noises and galloping rhythm can, along with PLG, be a sign of rheumatic aortic or mitral heart disease.
The most informative for the differentiation and diagnosis of lung scintigraphy, computed tomography and angiography. From laboratory tests, HIV-1 antibodies, liver and thyroid function tests are performed.
Methods of treatment
Treatment of PLG in most cases does not have much effect, it is possible to slightly increase the patient's life. As a rule, despite the ongoing therapy, the disease progresses and leads to a lethal outcome in 2-5 years.
The use of anticoagulants is prolonged and is shown to all patients without suffering from PLH.The use of drugs such as co-domadin, coumadin( warfarin), blood thinning and preventing the formation of blood clots, somewhat increases the survival rate.
With right ventricular failure prescribed cardiac funds, as well as diuretics, reducing peripheral edema.
To powerful modern drugs that are effective but do not increase survival statistics, endogenous vasodilators: prostaglandin I2( epoprostenol) can be reliably included. Long-term therapy with this drug can double the waiting period for transplantation, as well as increase the patient's life.
The safest means to relieve the general condition of the patient and reduce pressure, are drugs such as diazoxide, nitroglycerin, nitroprusside, apressin.
In patients with PGD, the use of such drugs as:
- b-agonists: isoproterenol, zatachaline;
- a-adrenoblockers: phenoxybenzamine, phentolamine;
- calcium channel blockers - long-term treatment with these drugs improves hemodynamics and survival;
Despite the high risk of transplantation, the most effective method of treatment is heart and lung transplantation.



