Altitude sickness: what is it, causes, symptoms, treatment
Content
- general information
- At what altitude does altitude sickness occur?
- How does altitude sickness occur?
- Who is affected by high-altitude hypoxia?
- How common is the disease?
- Symptoms and Signs
- Mild symptoms
- Moderate symptoms
- Severe symptoms
- Causes
- Diagnostics
- Treatment of high-altitude hypoxia
- Descent to a lower altitude
- Drug treatment
- Portable hyperbaric chambers
- Complications
- High-altitude cerebral edema
- High-altitude pulmonary edema
- Prevention and recommendations
general information
Altitude sickness (high-altitude hypoxia), also known as acute mountain sickness, is a potentially life-threatening condition. It occurs when a person is exposed to high altitude without acclimatization (i.e. gradually getting used to higher altitude).
Altitude sickness is caused by a drop in air pressure, making breathing difficult. Other common symptoms include:
- headache;
- nausea;
- dizziness;
- exhaustion.
In severe cases, altitude sickness can cause pulmonary edema (fluid in the lungs) and cerebral edema (fluid in the brain). This condition is very serious and requires immediate medical attention.
At what altitude does altitude sickness occur?

In its mildest form, altitude sickness can occur at about 2,500 m (8,000 ft) above sea level, which is the usual altitude for many ski resorts. However, more severe symptoms of altitude sickness occur at 3,600 m (about 12,000 ft) and higher.
How does altitude sickness occur?
As you climb higher up the mountain, the percentage of oxygen in the atmosphere remains constant (21%). However, when atmospheric pressure decreases, we breathe in less oxygen. This means the body has to adapt to breathing with less oxygen.
Who is affected by high-altitude hypoxia?
There are no specific factors, such as age, gender, or physical condition, that make a person more likely to develop altitude sickness. Some people are affected, while others are less susceptible to this condition.
How common is the disease?
Altitude hypoxia is quite common among people who spend time at high altitudes, such as climbers and skiers. For example, at an altitude of over 3000 m (about 10,000 feet), approximately 75% of people will experience mild symptoms. symptoms above).
In Russia, you can easily face altitude sickness, because in our country there are many high mountains (mainly the Greater Caucasus, Ural Mountains, Altai, Verkhoyansk ridge).
Description of terms:
Spicy: Acute means onset suddenly or over a short period of time.
Oxygen: Oxygen is a colorless, odorless gas that makes up about 20% of the air we breathe.
Symptoms and Signs

Altitude sickness is common at high altitudes. The onset and severity of symptoms and the height at which they occur vary depending on:
- human,
- how quickly you get to a great height, and
- the amount of time spent at high altitude.
Mild symptoms
Symptoms of mild altitude hypoxia include:
- headache;
- nausea;
- dizziness;
- fatigue;
- loss of appetite;
- stomach upset;
- feeling insecure;
- shortness of breath;
- increased heart rate;
- difficulty sleeping
- feeling unwell.
The symptoms of altitude sickness are usually worse at night. If moderate altitude hypoxia occurs, the person can continue with normal activities. For example, if a person is hiking or climbing, you can continue climbing at a constant speed.
Symptoms usually develop between 12 and 24 hours at altitude and begin to subside after 48 hours as the body begins to acclimate (gets used to changes in atmospheric pressure).
Moderate symptoms
Symptoms of moderate altitude sickness include:
- severe headache;
- nausea and vomiting;
- rapid breathing;
- lack of coordination (ataxia).
You will find that normal activities are difficult and the symptoms can be eliminated only by taking special medications (see. Section "Treatment") and descending to a lower height.
Read also:Emphysema of the lungs: what is it, causes, symptoms and treatment
A good way to test if someone has mild altitude sickness is to ask the person to walk 10 steps in a straight line. If there are problems with coordination and the person is unable to walk straight 10 steps, he should immediately descend to a lower altitude.
Severe symptoms
Symptoms of severe high-altitude hypoxia include:
- worsening of the symptoms described above;
- persistent irritable cough;
- dyspnea (even during rest);
- gurgling sound in your chest (caused by fluid in your lungs);
- coughing up pink, frothy fluid (phlegm);
- awkwardness and difficulty walking;
- irrational behavior;
- double vision (diplopia);
- convulsions (seizures);
- drowsiness;
- confusion (caused by swelling of the brain or fluid in the brain).
A severe form of the disease is a medical emergency. A person with severe acute mountain sickness must descend at least 600 m (2000 ft) immediately.
Causes

Altitude hypoxia occurs due to too rapid ascent to an altitude of 2500 m or more. The body takes time to adjust to low air pressures and lower oxygen levels at high altitudes. This is known as acclimatization.
It usually takes one to three days for the body to get used to the change in altitude. If you don't spend enough time getting used to altitude before climbing to a higher altitude, there is a good chance of getting altitude sickness.
Altitude hypoxia is potentially very serious and can be life-threatening. It is the body's response to a reduction in the supply of oxygen to the muscles and brain.
The decrease in oxygen content makes the heart and lungs work harder, causing an increase in heart rate and breathing rate. In response, more red blood cells are secreted to carry more oxygen throughout the body.
The body's attempts to cope with a decrease in the amount of oxygen cause changes in the patient's body:
- the level of acidity of the blood changes;
- pressure in the lungs;
- electrolytes (salts);
- water-salt balance.
Description of terms:
Erythrocytes (red blood cells) are the most abundant cellular component in the blood, carrying oxygen throughout the body and removing carbon dioxide.
Diagnostics
Altitude changes have specific effects on the body, causing symptoms such as headache, nausea and dyspnea. Usually, the first signs of altitude sickness are:
- headache;
- rave;
- weakness;
- difficulty sleeping
- stomach upset.
If you experience these symptoms, stop climbing and descend to a lower altitude until the symptoms disappear completely.
The formal diagnosis of high-altitude hypoxia is based on a headache with one or more other symptoms, unless there is another probable cause and you have ascended at least 2500 m (8000 ft).
Treatment of high-altitude hypoxia
Because acute mountain sickness is potentially life-threatening, don't ignore its signs and symptoms. In the past, people died of altitude sickness without understanding or ignoring the signs.
If there is a very mild form of high-altitude hypoxia, continue to ascend, but make sure you do it gradually and at a constant speed. Warn friends and family that you are traveling, how you feel, even if you have mild symptoms.
If the signs are a little more pronounced, stay at your current height to allow the body to adjust.
- Do not engage in physical labor, sports.
- Drink plenty of fluids (not alcohol).
- Do not smoke.
- Relax until you feel better.
Descent to a lower altitude
If altitude sickness occurs, the best treatment is to descend to a lower altitude.
Read also:Symptoms and treatment of pneumonia in an adult
Descending 300 m (1000 ft) will improve symptoms of moderate altitude hypoxia, and spending 24 hours at that lower altitude will significantly improve symptoms.
Stay at this altitude until the symptoms are completely gone. After two to three days, your body will acclimate and your symptoms should disappear. At this point, you can start climbing again.
If you have a severe condition, descend 600 m (2000 ft) immediately. You must descend as soon as possible, because death can occur at any moment. If symptoms do not significantly improve at a lower altitude, continue to decrease until they improve.
Pure (100%) oxygen can be given to improve severe breathing problems caused by altitude sickness.
Drug treatment
- Painkillers.
Pain relievers such as paracetamol or ibuprofen can be used to treat altitude sickness headaches.
- Acetazolamide.
Acetazolamide (Diacarb) may help reduce the severity of symptoms of acute mountain sickness.
One of the consequences of altitude sickness is that it changes the chemical balance of the blood. Acetazolamide corrects the chemical balance of the blood and speeds up breathing.
Faster breathing allows more oxygen to be taken in, which helps minimize symptoms such as headache, nausea, and dizziness. This can be especially helpful at night.
Since acetazolamide is an unlicensed prescription-only drug from a general practitioner, you should consult your doctor before taking the drug. There are a number of minor side effects associated with acetazolamide, including:
- paresthesia (numbness or tingling of the face, fingers, or toes);
- polyuria (excessive urination);
- and in rare cases, blurred vision.
- Dexamethasone.
Dexamethasone can be very helpful in treating severe cases of high-altitude hypoxia such as cerebral edema.
Dexamethasone is a powerful steroid that reduces inflammation (swelling) in the brain. It is usually taken in a dose of 4 mg three times a day. Symptoms usually improve within 6 hours.
Dexamethasone is especially useful for "buying time" until it is safe to descend. For example, it can be used at night to relieve symptoms when descent is not possible or could be dangerous.
Dexamethasone is effective in treating this condition. If you go hiking in the mountains, it is best to take it with you for emergency use.
However, dexamethasone can cause side effects such as:
- stomach upset;
- euphoria (a state of excitement or delight);
- depression.
As with acetazolamide, you should consult your doctor before taking dexamethasone.
- Nifedipine.
Nifedipine is often used to treat high blood pressure (hypertension), and it may be helpful in treating altitude sickness, especially pulmonary edema.
Nifedipine reduces the narrowing of the pulmonary artery caused by edema, helping to relieve chest tightness and facilitate breathing.
The recommended dosage of nifedipine is 20 mg every 6 to 8 hours. Nifedipine can cause a sudden drop in blood pressure, so if you are taking it, do not get up too quickly from a lying or sitting position.
Portable hyperbaric chambers
Portable hyperbaric chambers are often used to treat altitude sickness. You are inside the chamber and it fills with air, increasing the amount of oxygen inside. The processing effect is equivalent to a descent of 2000 m (6500 ft). Treatment should be continued for at least two hours, after which symptoms should improve significantly, allowing you to descend more safely.
Complications
Severe disease can lead to two very serious conditions known as:
- high-altitude cerebral edema;
- high-altitude pulmonary edema.
Read also:Pulmonary pleurisy: what is it, causes, symptoms and treatment
High-altitude edema is rare, but it can occur if a person rises too quickly to a very high altitude and stays there.
High-altitude cerebral edema
High-altitude cerebral edema occurs when a lack of oxygen causes fluid to leak through the capillary walls into the brain, causing brain tissue to swell. Capillaries are tiny blood vessels that surround major organs such as the brain, heart, and lungs.
Symptoms include:
- headache;
- weakness;
- disorientation;
- loss of coordination;
- loss of memory;
- hallucinations and psychotic behavior (inability to distinguish reality from imagination);
- loss of consciousness;
- to whom.
Cerebral edema can occur if a person stays at a very high altitude for a week or longer. If not treated immediately, it is likely that the condition will result in death. To prevent this, an immediate descent of at least 600 m (2000 ft) is required.
The steroid drug dexamethasone can be used to treat cerebral edema. However, a person with this condition should be admitted to the hospital as soon as possible in order to receive follow-up treatment.
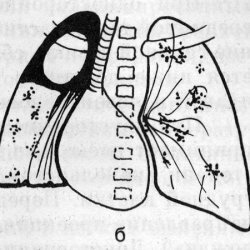
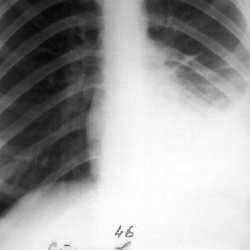
High-altitude pulmonary edema
High-altitude pulmonary edema occurs when fluid builds up in the lungs. The fluid prevents the transfer of oxygen from the lungs into the bloodstream. As the condition worsens, the amount of oxygen in the blood decreases, which causes the following symptoms:
- cyanosis (blue skin tone);
- severe breathing problems (even while resting);
- tightness in the chest (caused by a narrowing of the pulmonary artery);
- persistent cough, with discharge of a white foamy fluid (sputum);
- extreme tiredness and weakness;
- confusion and disorientation;
- irrational behavior;
- and finally death.
The symptoms of confusion and irrational behavior are associated with a lack of oxygen in the brain. To prevent death, a person with pulmonary edema must descend at least 600 m (2000 ft) immediately.
Nifedipine Is a medicine sometimes used to treat pulmonary edema. However, as with cerebral edema, a person with signs of pulmonary edema should be admitted to a hospital as soon as possible for follow-up treatment.
Prevention and recommendations
Before embarking on a mountaineering or trekking expedition, you need to be aware of the risks, symptoms, and treatments for high-altitude hypoxia.
NoteA: If you are traveling to a remote part of the world, it can be difficult to get medical care at the same level as in Russia.
- Acclimatization.
Proper acclimatization is the best way to prevent altitude sickness. Slow climbing will give your body time to adjust to the change in altitude.
Before booking your trip, make sure there is enough time to acclimate on your itinerary so you don't put yourself at unnecessary risk of illness.
- Sleep at a lower altitude.
When you exceed 3000 m, do not increase the altitude at which you sleep more than 300 m per night. You can climb higher during the day, but return every night to a camp that is no more than 300m higher than the previous night's camp.
If this is not possible, some travel companies include a day trip in the downhill trek to help acclimatize.
Some travel companies offer to climb the mountain in a short time, for example, climb Mont Blanc in a week. Climbing at this speed can lead to altitude sickness. It would be best to do this at the end of the two-week vacation after acclimatizing by climbing slightly lower peaks first.